Copy link
Vein of Galen Malformation
Last updated: 01/03/2025
Key Points
- The vein of Galen malformation (VOGM) is a rare congenital arteriovenous fistula that results in low-resistance intracranial circulation and downstream cardiopulmonary stress, including high-output heart failure and pulmonary hypertension.
- Endovascular embolization is the first line of treatment for VOGM, performed under general anesthesia.
- Anesthetic management is challenging due to the complex physiology of the VOGM, cardiac failure, and pulmonary hypertension.
Introduction and Pathophysiology
- The VOGM is a rare congenital arteriovenous fistula that arises from a failed regression of the median prosencephalic vein (MPV), a precursor to the vein of Galen (Figure 1). When the MPV fails to regress, high-pressure blood from the choroidal arteries is shunted into this low-pressure venous sac, which becomes aneurysmal. This leads to low-resistance intracranial circulation.
- In utero, the placental circulation provides a low-resistance sump that is thought to protect the fetal brain and heart from circulatory overload.1 With the loss of this placental sump after birth, volume overload to the right heart may ensue, leading to high-output heart failure and pulmonary hypertension.
- In the brain, venous hypertension may interfere with the absorption of cerebral spinal fluid and cause hydrocephalus and/or delayed developmental milestones. If left untreated, the condition is almost universally fatal owing to sequelae from the above-mentioned high-flow physiology.2
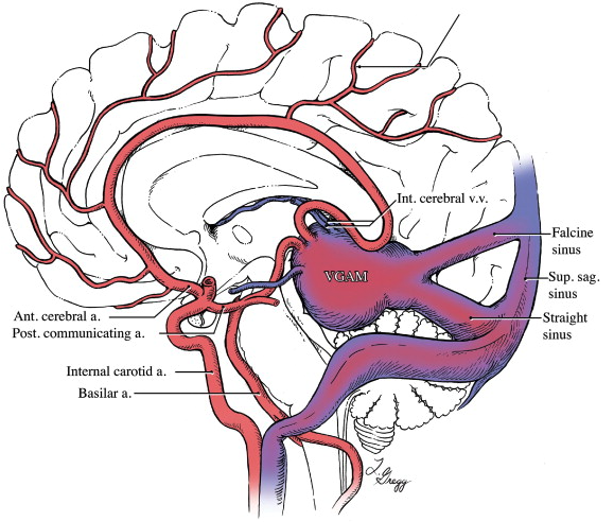
Figure 1. Anatomy relevant to the vein of Galen malformation. Used with permission from Pearl M et al. Cerebral venous development in relation to developmental venous anomalies and Vein of Galen aneurysmal malformations. Seminars in Ultrasound, CT, and MRI. 2011; 32 (3): 252-63. PubMed
Epidemiology
- The incidence of VOGM malformation has been estimated to be approximately 1:58,000 live births, representing the most frequently diagnosed fetal cerebrovascular anomaly.3
- Prenatal diagnosis is reported to occur in at least 29% of cases and is typically detected during the late 2nd or 3rd trimester by ultrasound.4
- VOGM is not associated with chromosomal aneuploidy or syndromic disease.
Clinical Presentation
- The age of clinical presentation will depend on aneurysmal complexity and flow characteristics.
- High-flow aneurysms composed of multiple arterial feeders and low outflow restriction tend to present with congestive heart failure in the neonatal period, often in the first few days of life.
- Less complex aneurysms with fewer feeders may present later in infancy or childhood with hydrocephalus, unusually prominent veins on the face/scalp, developmental delay, and/or persistent headache.
Diagnostic Radiography
- The diagnosis of VOGM is most often identified on antenatal ultrasound, where the dilated MPV appears as a posterior midline anechoic structure with prominent flow on Doppler (Figure 2). Antenatal echocardiograms may reveal fetal cardiomegaly, increased flow through the pulmonary artery, and retrograde diastolic flow through the isthmus of the aorta.5
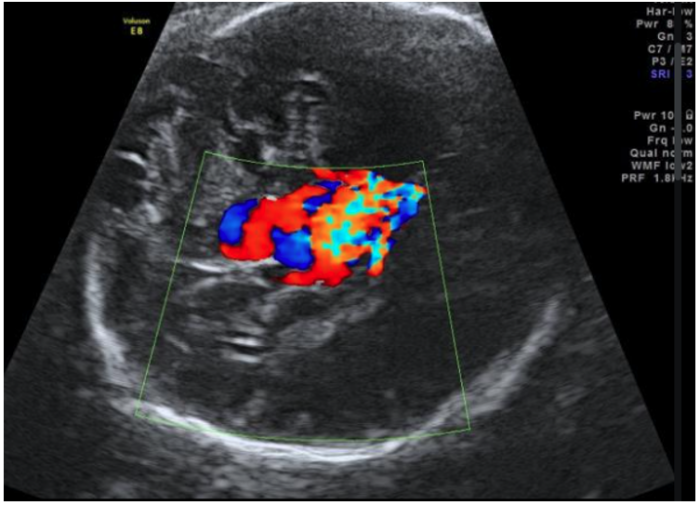
Figure 2. Ultrasound image showing a prominent anechoic midline structure within the fetal head. Doppler assessment demonstrates turbulent flow with a low resistance waveform. Source: Gaillard F. Vein of Galen malformation. Radiopaedia.org. April 25th, 2013. Accessed November 9th, 2024. Link
- Imaging by magnetic resonance angiography may follow the initial diagnosis by ultrasound to better delineate the feeding and draining vessels5 (Figure 3).
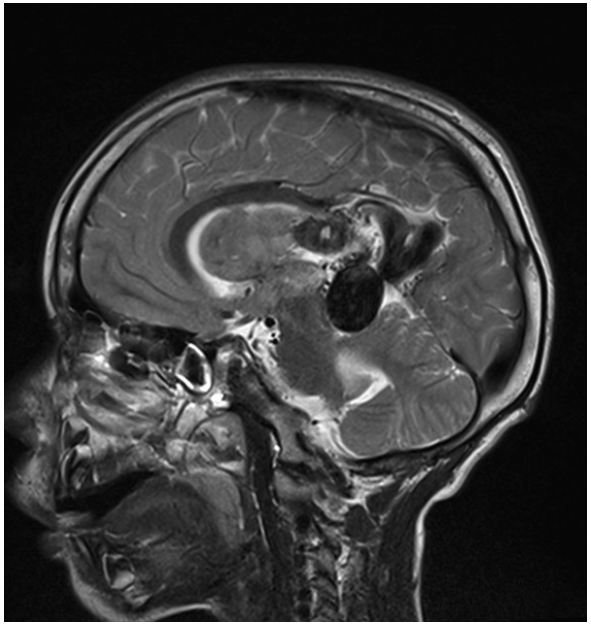
Figure 3. Magnetic resonance angiography demonstrating large arteriovenous malformations in the left parietal lobe with multiple vessels draining into the vein of Galen and straight sinus. The main arterial supply is from the left anterior cerebral artery. Hydrocephalus with significant intraventricular hemorrhage is also seen in both lateral ventricles, extending into the third and fourth ventricles. Source: Gaillard F. Vein of Galen malformation. Radiopaedia.org. April 25th, 2013. Accessed November 9th, 2024. Link
- Digital subtraction angiography (DSA) remains the gold standard for fully characterizing the lesion. It may reveal a spherical or ellipsoid varix that drains into the straight, transverse, and transverse/sigmoid sinuses5 (Figure 4).
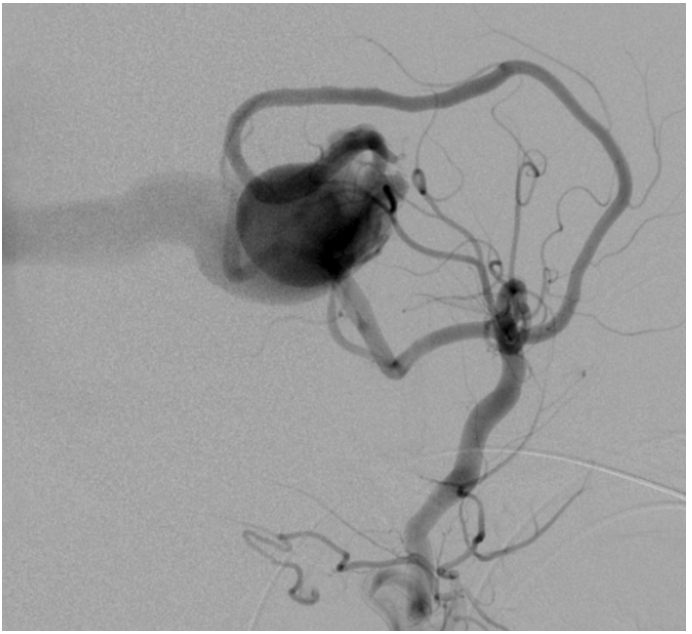
Figure 4. Digital subtraction angiography demonstrating vein of Galen malformation filling via branches of the posterior communicating artery, right posterior cerebral artery, and bilateral anterior cerebral arteries. Source: Gaillard F. Vein of Galen malformation. Radiopaedia.org. April 25th, 2013. Accessed November 9th, 2024. Link
Treatment and Prognosis
- The first-line treatment of VOGM involves endovascular embolization of arterial feeders and/or venous drains using coils or acrylic glue. This procedure is performed under general anesthesia and often occurs in stages. Multiple rounds of embolization are usually required to sufficiently decrease volume overload on the right heart.
- About a third of newborns with VOGM do not suffer acute postnatal cardiopulmonary decompensation and may be discharged from the neonatal intensive care unit (NICU) with plans for outpatient embolization. The remaining two-thirds of patients who do decompensate after birth will require urgent embolization.6
- Embolization is a high-risk but necessary procedure, as the prognosis for VOGM patients is primarily determined by the presence or absence of cardiac failure. The resolution of pulmonary hypertension is also an important indicator associated with survival and a surrogate endpoint for benchmarking outcomes in this population.7
- Despite advances in endovascular techniques, there remains a high rate of morbidity and mortality in this population, especially among patients with prenatally diagnosed VOGM with concurrent cerebral and cardiac anomalies.8
Anesthetic Considerations
- Preoperative workup should include reviewing the above-mentioned radiographic studies and an echocardiogram, with attention paid to the degree of pulmonary arterial pressure, presence of a ductus arteriosus, and/or presence of other structural anomalies such as an atrial septal defect or aortic coarctation. Laboratory tests evaluating hepatorenal function and coagulopathy should also be reviewed.
- Anesthetic management is challenging due to the complex physiology of VOGM, cardiac failure, and pulmonary hypertension. Patients may be on inotropes, diuretics, inhaled nitric oxide, and/or prostaglandins and will require high-risk transport from the NICU, often already intubated/sedated.
- General anesthesia is required and may be achieved through a careful intravenous and/or inhalational induction followed by maintenance using easily titratable agents, such as a combination of low-dose volatile and short-acting opioids. A total intravenous anesthetic may also be employed, especially when the use of a NICU ventilator does not allow for the administration of volatile agents.9
- Anesthetic and vasoactive medications should be selected to support right heart function, and paralysis with controlled mechanical ventilation is vital to ensure head immobility. VOGM, by itself, is not associated with a difficult airway, and the usual considerations for neonatal/infant airway management apply.
- Arterial access is often necessary for hemodynamic monitoring and should be performed according to the interventionalist’s access plan. Most commonly, endovascular access is achieved through the umbilical or femoral artery, which may preclude using these sites for hemodynamic monitoring. Following vascular access, the interventionalist will likely request heparin titrated to activated clotting time.
- Brief periods of apnea may be requested during DSA runs.
- Over the course of the case, one should expect a relatively large amount of fluid to be administered, as is necessary for catheter flushing, contrast injection, and embolic material delivery. This high fluid load can become problematic in the setting of heart failure, and postembolization care often involves aggressive diuresis.
- Uncontrolled hypertension during endovascular embolization, coupled with the high turbulent flow characterizing these arteriovenous shunts, may cause the glue to migrate further than intended, resulting in cerebral ischemia.10 As with other cerebral arteriovenous malformations (AVMs), there is a risk of reperfusion injury from increased cerebral blood flow once the shunt is closed, along with intracranial hemorrhage secondary to AVM rupture.
- Patients should recover in an intensive care unit, where follow-up imaging can be pursued to assess changes in vascular architecture and brain parenchyma, and cardiac function should be monitored.
References
- Smith A, Abruzzo T, Mahmoud M. Vein of Galen malformation and high-output cardiac failure. Anesthesiology. 2016;125(3):597. PubMed
- Alvarez H, Garcia Monaco R, Rodesch G, et al. Vein of Galen aneurysmal malformations. Neuroimaging Clin N Am. 2007; 17 (2):189–206. PubMed
- Brevis Nuñez F, Dohna-Schwake C, Epidemiology, diagnostics, and management of vein of Galen malformation. Pediatr Neurol. 2021; 119:50–5. PubMed
- Mortazavi M, Griessenauer C, Foreman P, et al. Vein of Galen aneurysmal malformations: a critical analysis of the literature with a proposal of a new classification system. J Neurosurg Pediatr. 2013;12 (3):293–306. PubMed
- Gaillard F. Vein of Galen malformation. Radiopaedia.org. April 25th, 2013. Accessed November 9th, 2024. Link
- Gopalan V, Rennie A, Robertson F, et al. Presentation, course, and outcome of postneonatal presentations of vein of Galen malformation: a large, single-institution case series. Dev Med Child Neurol. 2018; 60:424–9. PubMed
- Khurana J, Orbach DB, Gauvreau K, et al. Pulmonary hypertension in infants and children with Vein of Galen malformation and association with clinical outcomes. J Pediatr. 2023; 258 (7):113404. PubMed
- Deloison B, Chalouhi GE, Sonigo P, et al. Hidden mortality of prenatally diagnosed vein of Galen aneurysmal malformation: a retrospective study and review of the literature. Ultrasound Obstet Gynecol. 2012; 40:652–8. PubMed
- Hrishi AP, Lionel KR. Periprocedural management of Vein of Galen aneurysmal malformation patients: An 11-Year experience. Anesth Essays Res. 2017;11(3):630-635. PubMed
- Bhatia K, Mendes Pereira V, Krings T, et al. Factors contributing to major neurologic complications from a vein of galen malformation embolization. JAMA Neurol. 2020; 77(8):992-9. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.