Copy link
Syndrome of Inappropriate Antidiuretic Hormone Secretion and Cerebral Salt-Wasting Syndrome
Last updated: 07/02/2025
Key Points
- Hyponatremia is one of the most common electrolyte disturbances in the perioperative period and can be associated with myriad pathologies.
- Differentiating the syndrome of inappropriate antidiuretic hormone secretion (SIADH) from cerebral salt-wasting (CSW) syndrome is crucial, as their treatments differ significantly.
- For SIADH, the treatment typically involves fluid restriction, whereas for CSW syndrome, the treatment includes volume and salt replenishment.
Syndrome of Inappropriate Antidiuretic Hormone (SIADH) Secretion
Introduction
- SIADH is the most common cause of hyponatremia, which is the most common electrolyte disorder in hospitalized patients.
- SIADH is characterized by the excess release of antidiuretic hormone (ADH), regardless of plasma osmolality or hemodynamic triggers.1
• The primary causes of SIADH include malignancies (primarily small cell lung cancer), pulmonary diseases, central nervous system (CNS) disorders/insults, and various medications.2
• SIADH occurs more frequently than cerebral salt wasting in the setting of CNS disease.
• The clinical manifestations of SIADH vary based on how quickly hyponatremia develops, as well as its severity and chronicity. In cases of acute SIADH (less than 48 hours), symptoms develop due to cerebral edema and can range from mild, nonspecific signs such as weakness and headache, to severe, life-threatening conditions like seizures and coma.1,3
• Importantly, anesthesia and surgery represent additional factors relevant to SIADH development in the perioperative setting. Both are potent physiological stressors that can stimulate ADH release through non-osmotic and nonhemodynamic pathways.4 Consequently, anesthesiologists must remain vigilant for SIADH as a potential cause of postoperative hyponatremia.
Pathophysiology
Enhanced ADH secretion
- CNS disorders, including subarachnoid hemorrhage, traumatic brain injury, stroke, infections, and neoplasms, can directly stimulate the hypothalamic-pituitary axis, resulting in unregulated ADH release. This excessive ADH secretion occurs independently of normal osmotic or hemodynamic triggers, resulting in water retention, serum sodium dilution, and the production of inappropriately concentrated urine.3 Ectopic ADH production, most notably from small cell lung carcinoma, can also cause the syndrome.
Pulmonary and Ventilatory Triggers
- Pulmonary diseases, including pneumonia (bacterial, viral, or tuberculous), acute respiratory failure, asthma, atelectasis, and pneumothorax, are recognized causes of SIADH. Though the precise mechanism is unclear, these conditions may stimulate ADH release through hypoxia-related pathways or direct pulmonary afferent signaling.
- Importantly, positive pressure ventilation (PPV) contributes to the development of SIADH. PPV can activate pulmonary venous baroreceptors that sense a reduction in effective circulating blood volume, thereby leading to non-osmotic stimulation of ADH secretion and promoting water retention and hyponatremia.4
Drug-Induced SIADH
- Numerous medications can precipitate SIADH by enhancing ADH release or potentiating its renal effects. Common offenders include carbamazepine, oxcarbazepine, cyclophosphamide, selective serotonin reuptake inhibitors, and chlorpropamide. Certain chemotherapeutic agents, opioids, and NSAIDs have also been linked to inappropriate ADH activity.1
Surgical Stress and Hormone-Related Causes
- Surgery is another potent stimulus for ADH hypersecretion, likely mediated by pain and physiological stress.
- Hormonal disorders such as hypopituitarism or hypothyroidism can mimic SIADH, as can exogenous administration of vasopressin, desmopressin, or oxytocin.2
Renal Mechanisms
- ADH binding to vasopressin-2 (V2) receptors in the renal collecting ducts increases the expression of aquaporin-2 channels, promoting water reabsorption. This results in water retention, low serum osmolality, and urine that remains inappropriately concentrated despite hyponatremia.
- In hereditary SIADH, gain-of-function mutations in V2 receptors cause constitutive receptor activation, leading to persistent water absorption and hyponatremia resistant to standard treatments.4
Diagnosis
SIADH should be suspected in patients with hyponatremia in the setting of CNS injury, especially when the following criteria are met.3,5
- Hyponatremia (serum sodium 135 mEq/L or lower)
- Low plasma osmolality (less than 275 mosmol/kg)
- Inappropriately concentrated urine (urine osmolality more than 100 mosmol/kg)
- Elevated urine sodium (more than 40 mEq/L) in the absence of diuretics
- Clinical euvolemia (no signs of hypovolemia or edema)
- Normal thyroid, adrenal, and renal function
- Serum uric acid less than 0.24 mmol/L
- Serum urea less than 3.6 mmol/L, low normal serum creatinine
Treatment
- The cornerstone of SIADH management is fluid restriction and addressing the underlying cause.2,3 This is followed by the implementation of measures to correct sodium levels at a safe rate.4
- If there is no evidence of severe or moderate symptoms, treatment includes
- Fluid restriction (typically less than 1000-1500 mL/day)
- Discontinue causative agents
- Consider oral salt tablets or furosemide as a second line if hyponatremia is not corrected.
- Urea or tolvaptan for refractory cases
- In the presence of severe symptoms, moderately severe symptoms, or if the patient is at high risk for progression or intracranial disease, treatment includes
- Fluid restriction and administration of hypertonic saline (3% NaCl) cautiously
- Hyponatremia correction goal: 4–6 mmol per liter within 1–2 hours.1
- Correction limit: Low risk for Osmotic Demyelination Syndrome (ODS): 10 mmol per liter within the first 24 hours, 18 mmol per liter within the first 48 hours
- High risk for ODS: 8 mmol per liter during any 24-hour period
- Frequent monitoring of serum sodium (every 2-4 hours initially)
Cerebral Salt-Wasting Syndrome
Introduction
- Cerebral salt-wasting (CSW) syndrome is another potential cause of hyponatremia in the setting of CNS disease. CSW syndrome is characterized by the renal loss of sodium, leading to hyponatremia with elevated urine sodium and hypovolemia.6,7
- Among patients with CNS disease affected by hyponatremia, CSW syndrome occurs less frequently than SIADH. The true incidence of CWS syndrome is unclear, with studies suggesting 7-25% in patients suffering from hyponatremia after CNS pathology.6,7,8
Pathophysiology
- CSW syndrome can occur with any CNS insult but is most commonly described following subarachnoid hemorrhage (SAH). There are currently two main theories regarding the pathophysiology of CSW syndrome:
1) Natriuretic factors, primarily brain natriuretic peptide (BNP), are secreted by the brain following CNS injury. These peptides dampen sympathetic tone and induce sodium loss (natriuresis) by inhibiting sodium reabsorption in the renal tubules and reducing renin release.6,8,9
2) Adrenergic dysregulation: an initial adrenergic surge following CNS injury may contribute to acute vasoconstriction and pressure natriuresis, followed by a later reduction in sympathetic tone. This impaired sympathetic renal input is thought to contribute to reduced sodium resorption and impaired release of renin and aldosterone.7,8,10
Diagnosis
- CSW syndrome generally occurs within the first 7-10 days following CNS injury and is characterized by the following:6,7,8,11
- Hyponatremia (serum sodium 135mEq/L or lower)
- Elevated urine osmolality (more than 100 mosmol/kg) with elevated urine sodium (more than 40mEq/L)
- Clinical signs of hypovolemia (low central venous pressure, inferior vena cava collapsibility on ultrasound, signs/symptoms of dehydration)
- Low serum uric acid (less than 2mg/dL) and elevated fractional excretion of uric acid (more than 10%)
Treatment
- Differentiating SIADH from CSW syndrome as a cause for hyponatremia is crucial to appropriate treatment (see section below, “Differentiating SIADH from CSW” syndrome), as the respective therapies are very different. In CSW syndrome, the crux of therapy is volume and sodium repletion.
- If serum sodium is more than 125mEq/L, consider starting with isotonic fluids (i.e., 0.9% sodium chloride)
- If serum sodium is less than 125mEq/L and/or the patient is exhibiting signs and symptoms of severe hyponatremia:
- Start 3% hypertonic saline
- To mitigate complications from rapid serum sodium shifts, such as central pontine myelinolysis, avoid raising serum sodium faster than 4-6mEq/L per day6,8
- Monitor serum sodium frequently (every 1-2 hours) for the first 6-12 hours
- Consider the addition of fludrocortisone 0.1-0.4mg/day in divided doses for those with CSW syndrome unresponsive to the above therapies12
Differentiating SIADH from CSW syndrome
- Differentiating SIADH from CSW syndrome is crucial, as their treatments differ significantly. For SIADH, the treatment typically involves fluid restriction, whereas for CSW syndrome, the treatment includes volume and salt replenishment.
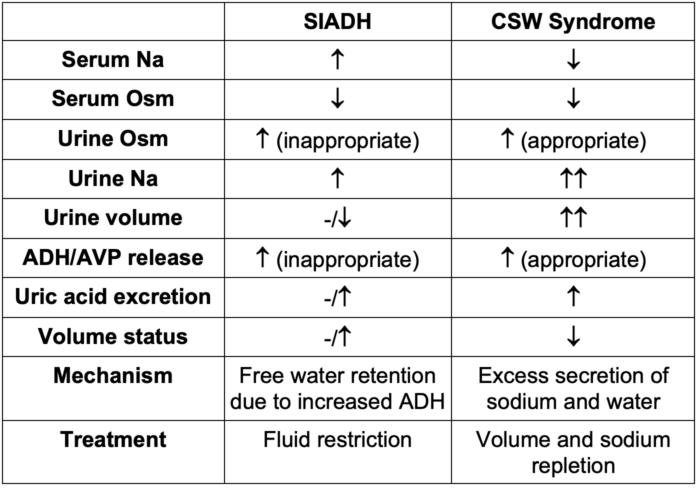
Table 1. Clinical comparisons between SIADH and CSW syndrome. Abbreviations: Na, Sodium; Osm, osmolality; ADH, antidiuretic hormone; AVP, arginine vasopressin
Anesthetic Considerations
- Hyponatremia is one of the most common electrolyte disturbances and can be associated with myriad pathologies. Often, patients with hyponatremia are asymptomatic and may require a high index of suspicion, especially in cases of chronic hyponatremia. However, CNS injuries should raise concern for potential electrolyte abnormalities, specifically sodium dysregulation. While SIADH accounts for the majority of cases of hyponatremia due to CNS insult, CSW syndrome must be differentiated, as their treatments are very different.
Preoperative Evaluation
- Recognize that certain procedures and pathologies are associated with a higher risk of hyponatremia and/or CNS injury:
- Trauma/head injury
- Neurosurgical procedures
- Stroke
- Intracranial pathologies: hemorrhage, tumor
- Meningitis
- Evaluate the patient for signs/symptoms of hyponatremia. Recall that chronic hyponatremia may present with more insidious changes than acute hyponatremia:
- Altered mental status
- Gait disturbances
- Nausea or vomiting
- Fatigue
- Headache
- Severe (serum Na less than 115meq/L): loss of consciousness, seizures, coma, death
- Laboratory values concerning for hyponatremia
- Serum sodium 135mEq/L or lower
- Serum osmolality 280mosmol/kg or lower
- Attempt to determine the underlying pathogenesis responsible for hyponatremia before surgery, if able (i.e., SIADH, CSW syndrome, renal losses, adrenal insufficiency). Please see the OA summary on hyponatremia for more details. Link
- Additionally, determining the severity and chronicity of the hyponatremia will help identify and guide appropriate treatment.
- If surgery is elective, consider rescheduling after medical optimization
- If surgery is urgent or time-sensitive, consider initiating treatment in the preoperative area and optimizing as much as possible prior to the procedure
- If surgery is emergent, proceed with surgery and attempt to correct hyponatremia intraoperatively
Intraoperative Management
- Monitors and lines
- In addition to standard American Society of Anesthesiologists monitors, consider using an arterial line for close hemodynamic monitoring and laboratory draws.
- Ensure adequate intravenous or central access in case the patient requires large-volume resuscitation or vasopressor support.
- In patients with altered mental status, the use of intraoperative electroencephalography monitoring can be useful to mitigate anesthetic overdose (as hyponatremia is thought to reduce anesthetic requirement).
- Induction
- Patients who suffer from hypovolemic hyponatremia may be at a higher risk for hemodynamic instability with induction. If the patient requires volume, recommend starting this resuscitation in the preoperative setting if possible.
- Consider etomidate, ketamine, or judicious pressor usage on induction to minimize hypotension
- Patients who present with nausea and vomiting from hyponatremia may benefit from rapid sequence induction (RSI) if there are no other contraindications.
- Fluid Management
- Fluid management should be largely guided by the underlying pathology of the hyponatremia and the patient’s volume status.
- In SIADH, fluid restriction is the primary treatment strategy.
- CSW syndrome benefits from fluid resuscitation with isotonic or hypertonic saline.
- Caution should be taken not to correct the serum sodium quicker than 4-8mEq/L per day (or 0.7mEq/L/h) to avoid central pontine myelinolysis.6
- In general, hypotonic fluids should be avoided for patients with hyponatremia.
Postoperative Management
- An intensive care unit should be considered for closer hemodynamic and electrolyte monitoring postoperatively.
- Serum sodium should be closely monitored until corrected.
- Volume status should also be monitored to assess the need for ongoing fluid resuscitation.
References
- Adrogué HJ, Madias NE. The syndrome of inappropriate antidiuresis. N Engl J Med. 2023;389(16):1499-1509. PubMed
- Verbalis JG, Greenberg A, Burst V, et al. Diagnosing and Treating the Syndrome of Inappropriate Antidiuretic Hormone Secretion. Am J Med. 2016;129(5):537.e9-537.e23. PubMed
- Ellison DH, Berl T. Clinical practice. The syndrome of inappropriate antidiuresis. N Engl J Med. 2007;356(20):2064-72. PubMed
- Jones DP. Syndrome of inappropriate secretion of antidiuretic hormone and hyponatremia. Pediatr Rev. 2018;39(1):27-35. PubMed
- Hoorn EJ, van der Lubbe N, Zietse R. SIADH and hyponatraemia: why does it matter? NDT Plus. 2009;2(Suppl_3):iii5-iii11. PubMed
- Hall WA, Thorell W. Cerebral salt wasting syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Link
- Cerdà-Esteve M, Cuadrado-Godia E, Chillaron JJ, et al. Cerebral salt wasting syndrome: review. Eur J Intern Med. 2008;19(4):249-54. PubMed
- Dholke H, Campos A, Reddy CN, Panigrahi MK. Cerebral salt wasting syndrome. J Neuroanaesthesiol Crit Care 2016; 3:205-10. Link
- Leonard J, Garrett RE, Salottolo K, Slone DS, Mains CW, Carrick MM, Bar-Or D. Cerebral salt wasting after traumatic brain injury: a review of the literature. Scand J Trauma Resusc Emerg Med. 2015;23:98. PubMed
- Singh S, Bohn D, Carlotti A, Cusimano M, et al. Cerebral salt wasting: Truths, fallacies, theories, and challenges. Critical Care Medicine. 2002; 30(11): 2575-9. PubMed
- Sterns R, Rondon-Berrios H. Cerebral salt wasting is a real cause of hyponatremia: CON. Kidney360. 2023; 4(4): e441-4. PubMed
- Bhat R, Baldeweg SE, Wilson SR. Sodium disorders in neuroanaesthesia and neurocritical care. BJA Educ. 2022;22(12):466-73. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.