Copy link
Serotonin Syndrome
Last updated: 04/06/2023
Key Points
- Serotonin syndrome is a potentially life-threatening condition caused by excessive serotonin levels in the central nervous system (CNS). Serotonin syndrome is typically precipitated by the concomitant use of multiple serotonergic medications.
- Serotonin syndrome is a clinical diagnosis and manifests as a wide spectrum of clinical presentations, ranging from mild self-limiting symptoms to life-threatening autonomic dysfunction.
- Several routinely used anesthetic medications may interact with commonly prescribed serotonergic medications, increasing the risk of developing serotonin syndrome in the perioperative period.
- The clinical presentation of serotonin syndrome is similar to neuroleptic malignant syndrome, anticholinergic syndrome, malignant hyperthermia, and thyroid storm.
Pathophysiology
- Serotonin syndrome (or serotonin toxicity) typically occurs following the administration of two or more medications that increase serotonin levels. This leads to an excitatory state with excessive serotonin within synapses of the CNS.1
- Several antidepressant medications are known to increase systemic levels of serotonin, including monoamine oxidase inhibitors (MAOIs), selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), tricyclic antidepressants (TCAs), some opioids, antihistamines, serotonin-releasing illicit drugs, and over-the-counter herbal medications1 (Figure 1).
- Commonly used anesthetic medications that increase serotonin levels include ondansetron, metoclopramide, fentanyl, tramadol, meperidine, and methadone1 (Figure 1).
- The risk of developing serotonin syndrome is increased in patients taking MAOIs combined with a second MAOI or SSRI, SNRI, or TCA.1 Serotonin syndrome may rarely occur in patients on high-dose monotherapy of a serotonergic agent.
- TCAs, SSRIs, and SNRIs inhibit the cytochrome P-450 enzymes, and may impact the clearance of other medications metabolized by this pathway.
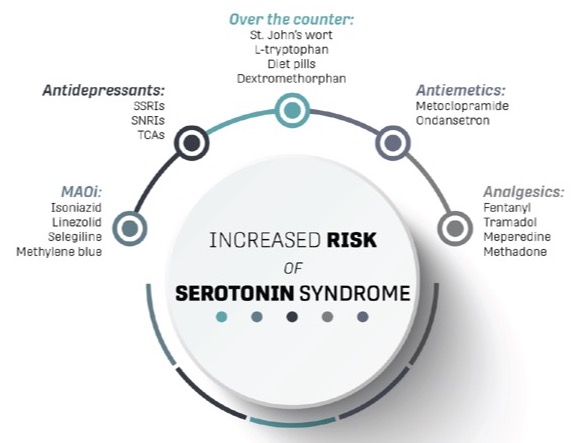
Figure 1. Medications associated with a risk of developing serotonin syndrome. Created by Sydney Yee, MD. Reprinted with permission.
Clinical Presentation & Diagnosis
- The classic presentation of serotonin syndrome includes a triad of altered level of consciousness (agitation, restlessness, confusion), autonomic dysfunction (hypertension, tachycardia, hyperthermia), and neuromuscular excitability (clonus, rigidity, hyperreflexia).2
- Symptoms range from mild self-limiting conditions to life-threatening hemodynamic instability3 (Figure 2).
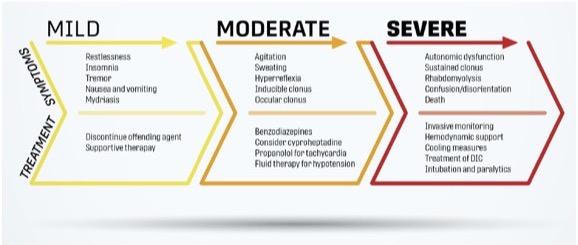
Figure 2. Range of clinical symptoms and treatment of serotonin syndrome. Created by Sydney Yee, MD. Reprinted with permission.
- Although several different criteria have been proposed for the diagnosis of serotonin syndrome, the Hunter Serotonin Toxicity Criteria is a validated tool widely used for the diagnosis of serotonin syndrome4 (Figure 3).
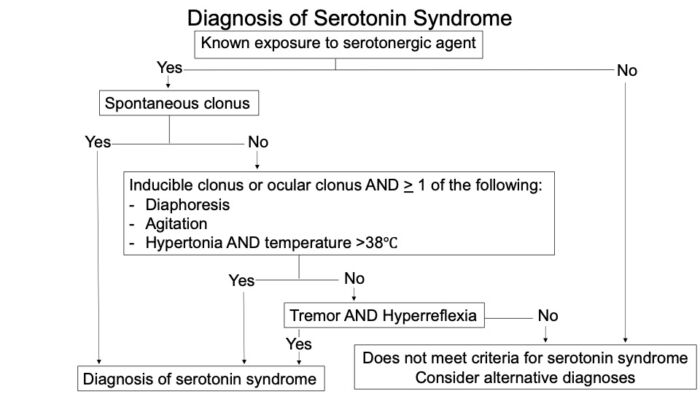
Figure 3. Hunter Serotonin Toxicity Criteria for diagnosis of serotonin syndrome. Adapted from Boyer EW. Serotonin syndrome (serotonin toxicity). In: Post T, ed. UpToDate. 2022.
Differential Diagnosis
- Serotonin syndrome is a diagnosis of exclusion, and has features similar to neuroleptic malignant syndrome, anticholinergic syndrome, malignant hyperthermia, and thyroid storm3 (Figure 4).
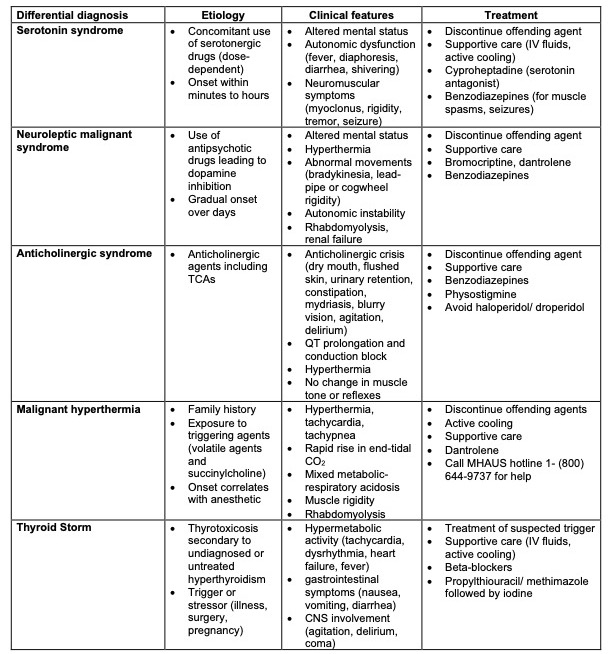
Table 1. Differential diagnosis of serotonin syndrome. (Abbreviations: MHAUS = Malignant Hyperthermia Association of the United States; IV = intravenous)
Anesthetic Considerations
- A physical examination should be performed and a thorough medical history obtained that elicits the use of herbal medications, illicit substances (LSD, ecstasy, cocaine, amphetamines), and psychotropic or serotonergic medications.
- Typically, antidepressants including SSRIs, MAOIs, TCAs, SNRIs, are continued throughout the perioperative period to avoid the recurrence of depression and precipitation of withdrawal symptoms. The same is true for antipsychotics, anxiolytics, and antiepileptic/mood stabilizer medications. The timing and dosage of these medications should be delineated to avoid the administration of multiple serotonergic agents in short succession.
- Due to interference of cytochrome P-450 clearance, benzodiazepines and neuromuscular blocking agents may have prolonged effects.
- For high-risk patients taking multiple serotonergic agents, administering hydromorphone rather than fentanyl, oxycodone, tramadol, or methadone for analgesia should be considered.3
- Meperidine for postoperative shivering should be avoided.
- Clinicians should avoid ondansetron and administer an alternate medication for postoperative nausea and vomiting prophylaxis.3
Management
- First-line management involves removing the offending agent and avoiding the administration of additional serotonergic agents.2
- Mild cases of serotonin syndrome may be safely managed with supportive care and observation. Monitoring in the postanesthesia care unit for a prolonged period (6 hours) should be considered to observe the resolution of symptoms.3
- Patients with moderate to severe serotonin syndrome should be admitted to the hospital with consultation from intensive care physicians and toxicologists. Agitation/restlessness may be managed with benzodiazepines. Tachycardia and hypertension may be controlled with propranolol (which also contains antiserotonergic properties).3
- Cyproheptadine is a specific serotonin antagonist that can lead to the rapid reversal of serotonin syndrome. Cyproheptadine is only available in oral form.2
References
- Foong AL, Grindrod KA, Patel T, et al. Demystifying serotonin syndrome (or serotonin toxicity). Can Fam Physician. 2018;64(10):720-7. PubMed
- Jones D, Story DA. Serotonin syndrome and the anaesthetist. Anaesth Intensive Care. 2005; 33 (2):181-7. PubMed
- Baldo BA, Rose MA. The anaesthetist, opioid analgesic drugs, and serotonin toxicity: a mechanistic and clinical review. Br J Anaesth. 2020; 124 (1): 44-62. PubMed
- Dunkley E, Isbister G, Sibbritt D, et al. The Hunter serotonin toxicity criteria: simple and accurate diagnostic decision rules for serotonin toxicity. QJM. 2003;96(9): 635-42. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.