Copy link
Rib Fractures: Pain Management
Last updated: 03/22/2023
Key Points
- Rib fractures can result in significant morbidity and mortality, especially multiple rib fractures, flail chest, elderly patients, and patients with chronic lung disease.
- Deterioration of pulmonary function can result from hypoventilation due to pain, impaired gas exchange, and altered breathing mechanics.
- Early pain service consultation, multimodal analgesia and regional anesthetic blocks improve patient outcomes.
Introduction
- Rib fractures are common injuries that can result in significant morbidity and mortality.
- The most common mechanism of injury is blunt chest trauma from motor vehicle accidents or falls (especially in elderly patients).1 Other less common etiologies include1
- Penetrating trauma
- Stress fractures from chronic coughing, athletes (golfers, rowers, throwers), etc.
- Pathological fractures from bony metastases from prostate, breast, or renal cancers
- Nonaccidental trauma in infants and young children
Anatomical Considerations
- All 12 pairs of ribs articulate posteriorly with the respective thoracic vertebrae and transverse vertebrae. The first seven ribs are true ribs as they articulate anteriorly with the sternum directly via costal cartilages. Ribs 8-10 are false ribs as their anterior attachments are not direct. Ribs 11 and 12 are floating ribs as they do not have an anterior attachment.
- Ribs 4-10 are most susceptible to fractures. The first three ribs are relatively protected by the clavicle and shoulder girdle. The floating ribs (11 and 12) are more mobile and less likely to fracture.
- Traumatic rib fractures usually occur at the site of impact or at the posterolateral bend, where the rib is the weakest.
- Ribs in children are more pliable and require a greater force to produce a fracture.
Flail Chest
- Radiographically, a flail chest refers to the presence of three contiguous ribs fractured in two or more places. Clinically, it results in paradoxical chest movement in a patient breathing spontaneously.
- It is usually associated with more severe injury and increased mortality.
Clinical Considerations
- The main concern is the deterioration of pulmonary function 24-72 hours after the injury through three primary mechanisms.2
- Pain causing ineffective cough and sputum retention can lead to hypoventilation and atelectasis. This has been shown to increase the likelihood of developing pneumonia, especially in elderly patients.1,2
- In patients with pulmonary contusions and potential hemorrhage, gas exchange is typically impaired due to the subsequent edema and reduced lung compliance. This leads to worsening hypoxemia, hypercarbia, and increased respiratory effort.1,2
- In patients with a flail chest, breathing mechanics may be altered. Displaced fractures may also damage surrounding lung structures leading to tears in the pleura and damage to intercostal vessels, possibly leading to pneumothorax and hemothorax.1,2
- Risk factors for developing complications following rib fractures include2
- Elderly patients older than 65 years
- Frailty or significant comorbidities
- Smokers and pre-existing chronic respiratory disease
- Prior use of anticoagulation
- Flail chest, pulmonary contusion, pneumothorax, or hemothorax
- Associated major trauma
- Clinical signs of lower respiratory infection
- Certain patterns of injury warrant additional evaluation.2
- Multiple rib fractures are usually associated with pulmonary contusions.
- Lower rib fractures (7-12) may be associated with abdominal injuries.
- A fracture of the first rib usually indicates a high-energy impact.
- A flail chest with displaced ribs may damage the underlying pleura or lung.
Initial Evaluation and Imaging
- The patient must be evaluated by a multidisciplinary trauma team. Early pain service consultation has been shown to improve outcomes.3
- The initial evaluation should include a detailed history of the mechanism of injury and the presence of associated comorbidities and other risk factors
- Physical examination should be focused on identifying any signs of respiratory compromise, such as hypoxia, inability to clear secretions, shallow breathing, flail segment, etc.2
- In addition to a chest x-ray, a computed tomography (CT) chest should be considered in high-risk patients. The overall sensitivity of chest x-rays for rib fractures is poor, and more than 60% of rib fractures are not detected on chest x-rays.1,2
- Complications such as pneumothorax, hemothorax, or pulmonary contusions should be ruled out.
- Multiple scoring tools have been developed, but they are unable to demonstrate consistent clinical utility.1
Management
Ventilatory Management
- Supplemental oxygen is often needed.
- Use of an incentive spirometer maintains alveolar recruitment and provides an objective assessment of pulmonary function.
- High-flow nasal cannula or noninvasive ventilation should be considered in patients who develop hypoxia and/or hypercarbia.
- Intubation and positive pressure ventilation may be necessary for some patients.
Pain Management Strategies
Multimodal analgesia is crucial in improving patient outcomes.3
Oral Medications
- Oxycodone pro ne nata (PRN) vs. scheduled
- Gabapentin 100-300mg TID, can consider up to 600mg TID in healthy patients, reduce dose in patients with renal impairment and monitor for sedation as a side effect
- Acetaminophen up to 3g/day
- Nonsteroidal anti-inflammatory drugs: 200 – 800mg TID, monitor kidney function and concern for platelet dysfunction and bleeding.
- Muscle relaxer: cyclobenzaprine 5-10mg TID or methocarbamol 750-1500mg TID.
- Tramadol or methadone can be considered in nonopioid-naïve patients with very poor pain control.
Parenteral Medications
- Intravenous (IV) opioids PRN: hydromorphone 0.2-0.4mg q2-4 hours
- IV opioid patient-controlled analgesia 0.1-0.2 mg/kg, consider fentanyl or hydromorphone in patients with impaired renal function
- IV ketamine: consider in nonopioid-naïve patients, caution in patients with liver dysfunction, pregnancy, and psychiatric history
Regional Blocks
- Several unilateral or bilateral blocks can be performed to cover specific regions based on the number and location of the fractures.1
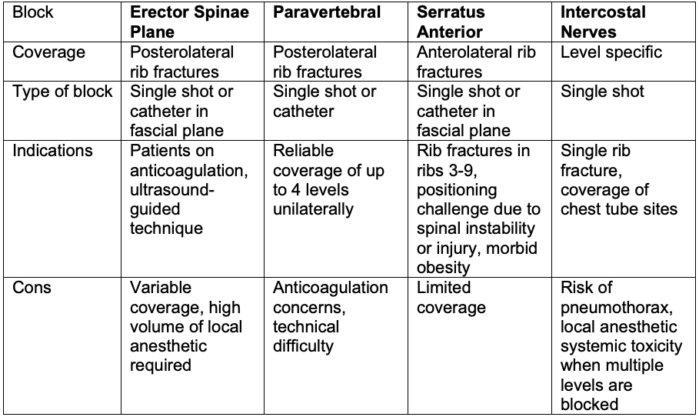
Table 1.
Thoracic Epidural
- Thoracic epidurals have the best evidence of efficacy for rib fractures. A systematic review and meta-analysis showed that a thoracic epidural catheter provides better pain relief than IV analgesia, paravertebral, and intercostal blocks.4 There was no difference in secondary outcomes such as the length of intensive care unit stay, mechanical ventilation, or pulmonary complications.
- A thoracic epidural catheter provides effective analgesia for 2-3 levels above and below the insertion site. However, it may be technically difficult to perform, and positioning may be challenging in some patients.1
- Epidurals are contraindicated in patients with coagulopathy or sepsis. Other concerns include hypotension, urinary retention, reduced mobility, spinal cord trauma, infection, and/or hematoma.1
Surgical Rib Fixation
- Surgical rib fixation is typically reserved for patients with flail chest who need mechanical ventilation.1 Other indications include severely displaced rib fractures with respiratory compromise, significant chest wall deformity, patient undergoing thoracotomy for other reasons, chronic malunion, failure to wean from mechanical ventilation, etc.
References
- Williams A, Bigham C, Marchbank A. Anaesthetic and surgical management of rib fractures. BJA Educ. 2020;20(10):332-40. PubMed
- Jeffery Z, Everson M, Carty S. Management of rib fractures. Br J Hosp Med (Lond). 2019;80(10):C146-9. PubMed
- Sborov KD, Dennis BM, de Oliveira Filho GR, et al. Acute pain consult and management is associated with improved mortality in rib fracture patients. Reg Anesth Pain Med. 2022; rapm-2022-103527. PubMed
- Peek J, Smeeing DPJ, Hietbrink F, et al. Comparison of analgesic interventions for traumatic rib fractures: a systematic review and meta-analysis. Eur J Trauma Emerg Surg. 2019;45(4):597-622. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.