Copy link
Rapid Sequence Induction and Cricoid Pressure
Last updated: 01/21/2025
Key Points
- Rapid sequence induction and intubation (RSII) is used for emergency situations or when a patient is at risk of pulmonary aspiration. It involves administering a rapid-acting sedative and neuromuscular blocking agent, followed by endotracheal intubation.
- RSII requires careful preparation, including preoxygenation, patient positioning, and having backup airway management options available in case of difficulty.
- RSII has potential complications, including hypotension, hypoxia, bradycardia, and aspiration. These risks can be mitigated through careful patient selection, appropriate medication dosing, and close monitoring of vital signs.
Introduction
- Pulmonary aspiration was the most common cause of anesthesia-related death in the 4th National Audit Project of the Royal College of Anaesthetists.1
- RSII is a widely used technique to secure an airway in patients with greater than normal risk for pulmonary aspiration.2
- During the routine induction of general anesthesia, there is a period between the loss of consciousness and inflation of the endotracheal tube cuff, during which airway protective reflexes are lost, and patients are at risk of aspiration.2
- RSII aims to achieve airway protection with a cuffed endotracheal tube as quickly as possible following induction of anesthesia to reduce this aspiration risk.2
Indications for RSII
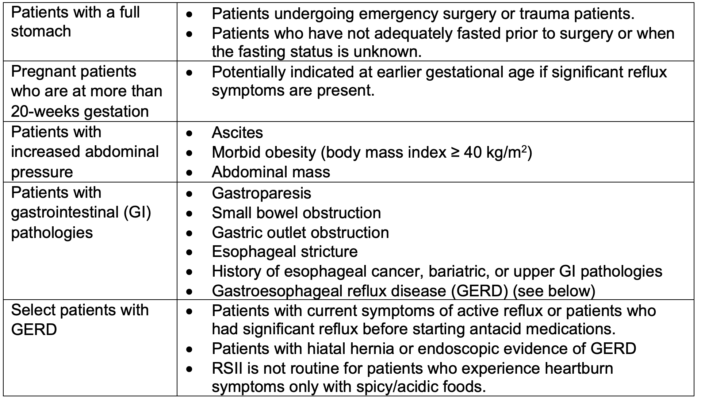
Table 1. Indications for RSII.2,5
Technique
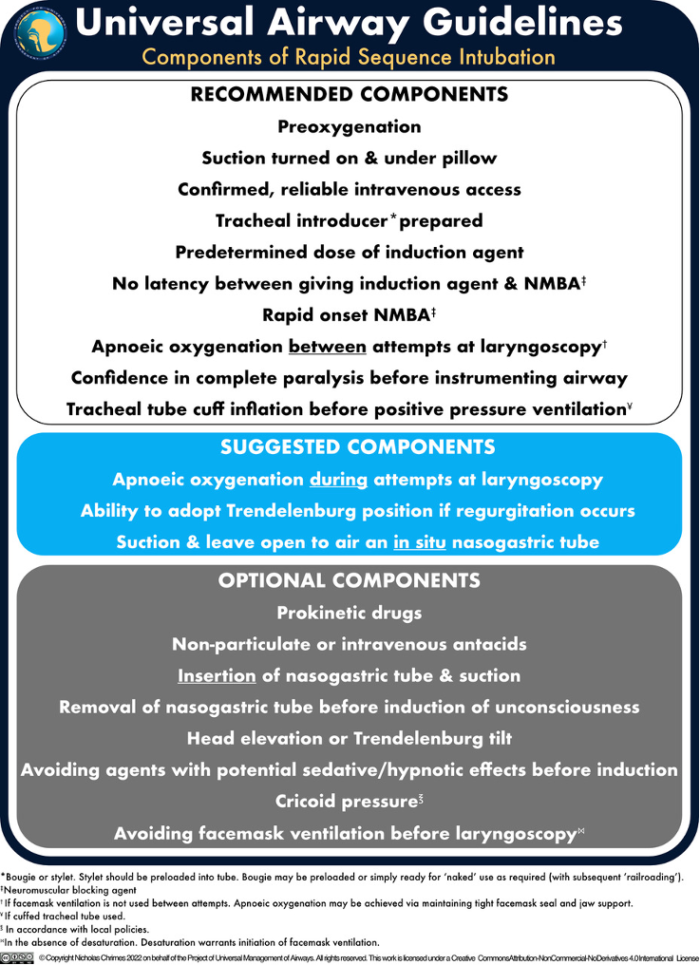
Figure 1. Protocol for RSII. Created by Nicholas Chrimes for the Project of Universal Management of Airways. Reprinted with permission.
Drugs
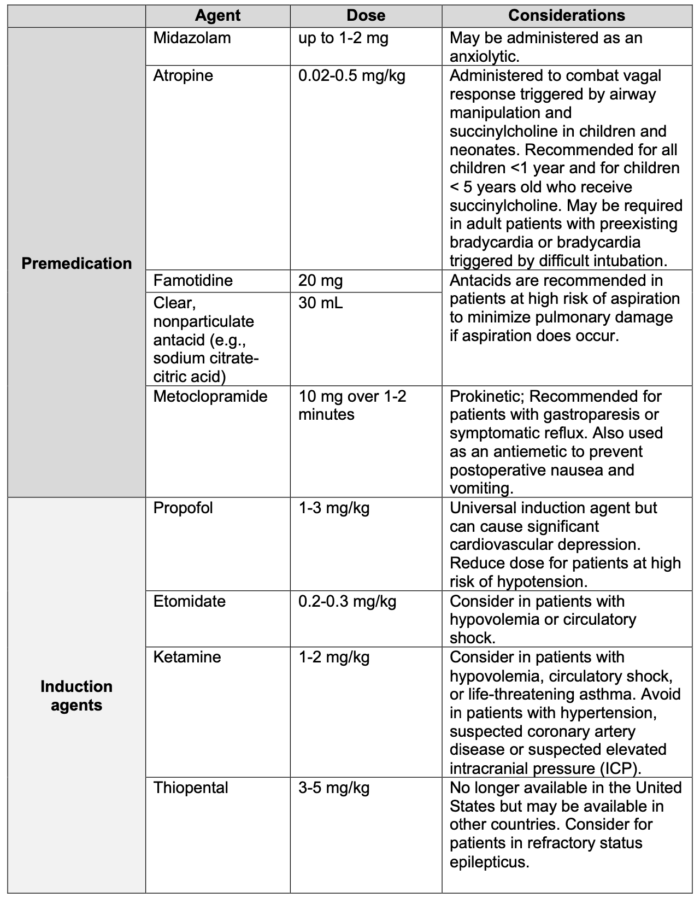
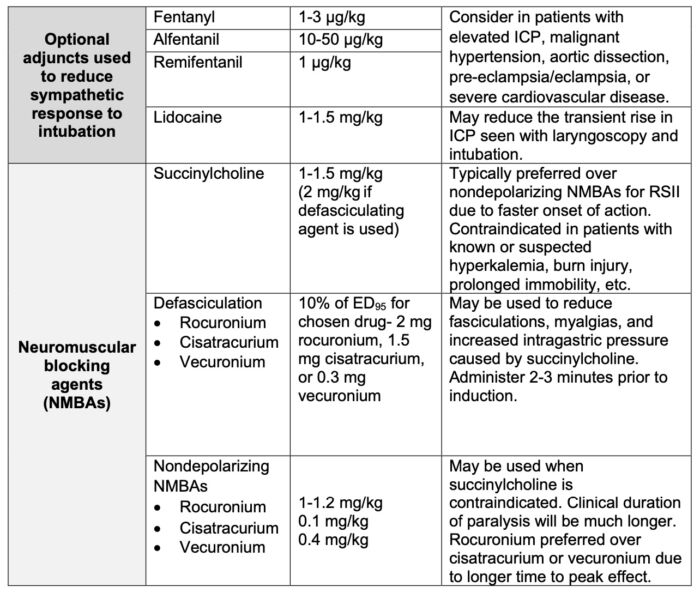
Table 2. Medications for RSII.2,5
Cricoid Pressure
- Cricoid pressure (CP), also known as the Sellick maneuver, was first described by Dr. Brian Sellick in 1961 as a means of preventing aspiration during induction of anesthesia. The technique has since become a standard component of RSII protocols, although its efficacy and optimal application remain a topic of debate.3
- CP involves applying pressure to the cricoid cartilage while intubation is performed to compress the esophagus against the vertebral column and prevent gastroesophageal reflux and subsequent aspiration. The most recommended technique for applying cricoid pressure during RSII involves using the thumb, index, and middle fingers; however, the thumb and index finger alone, or alternatively just the index and middle fingers, may be used instead. CP must be maintained until the endotracheal tube is properly in place and the cuff is inflated.3
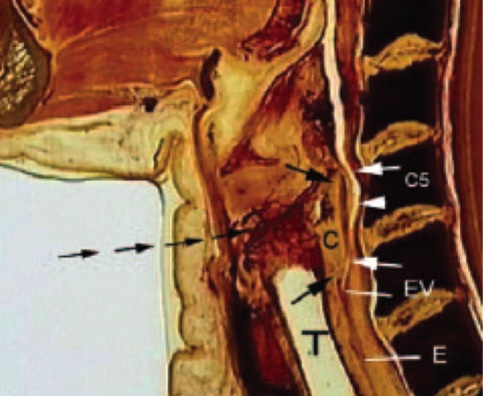
Figure 2. Anatomy of the neck at the level of the cricoid ring on sagittal cadaver image. The superior and inferior aspects of the cricoid cartilage (C) are indicated by black arrows. As pressure is applied anteriorly (multiple lines of black arrows), the cricoid cartilage is compressed against the C5 vertebral body sealing off the esophagus (E) at the esophageal verge (EV). Because the esophagus is well below the level of the seal, its position is irrelevant to the integrity of the seal produced by the pressure on the unit. Used with permission from Rice MJ, et al. Cricoid pressure results in compression of the postcricoid hypopharynx: the esophageal position is irrelevant. Anesth Analg. 2009; 109:1546-52.
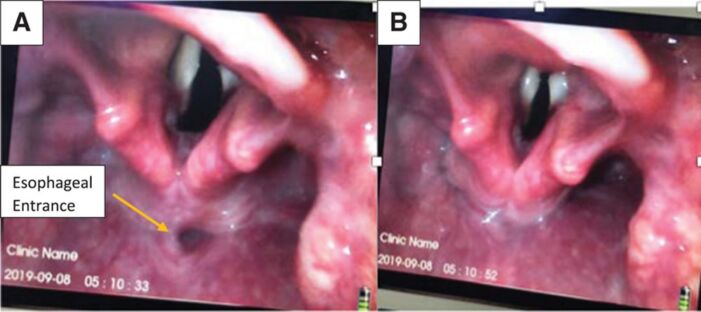
Figure 3. Esophageal entrance on video laryngoscopy (A) before application of CP and (B) after application of CP. Used with permission from Khorasani A, et al. Cricoid pressure: Do no harm but do It correctly; Anesth Analg. 2021;132(2): e20-e21.
- The use of CP in RSII is a controversial topic in the anesthesia community due to limited evidence supporting its efficacy and concerns about its impact on time to intubation and visualization of the airway. Additionally, in children and infants, airway patency may be compromised with over-excessive CP force due to increased compliance of the tracheal cartilage.3,5
- In the United States, the use of cricoid pressure has become a standard of care for RSII, in part due to concerns about malpractice litigation. However, in other countries, the use of cricoid pressure is more controversial and used less frequently.3
- Another key factor in the use of CP is the competence of the provider in performing the procedure correctly. Improper application of CP can interfere with intubation and increase the risk of complications. However, there is no consensus on the optimal technique for cricoid pressure, including the amount of force used, the location of pressure application, and the patient position.3
- Traditionally, the recommended amount of force for CP has been 30 Newtons (N), equivalent to approximately 3 kg of force.6 However, some studies have suggested that lower amounts of force may be sufficient to reduce the risk of aspiration while minimizing the potential for complications.7
- Ultimately, more high-quality scientific evidence is needed to determine the effectiveness and safety of CP.3
- Other methods that may be used in place of or in adjunct to cricoid pressure to prevent aspiration include nasogastric tube placement and gastric ultrasound to assess the volume of gastric contents.2,3
Potential Complications of RSII
1. Hypoxia
- Hypoxia is the most common complication of RSII, particularly in patients with limited pulmonary reserve (i.e., critically ill, pregnant/peripartum, or obese patients).2,5
- Desaturation may be prevented by ensuring adequate preoxygenation and using low-pressure (<20 cmH2O) mask ventilation during RSII in these patients.2
- Additionally, strategies to lengthen the time to apneic oxygen desaturation may include passive apneic oxygenation using high-flow oxygen through a nasal cannula or continuous positive airway pressure preoxygenation.2
2. Difficult or failed airway
- RSII is associated with an increased risk of difficulty in airway management.2
- Failed intubation occurs in 1 in 2,000 elective cases but increases to 1 in 300 for RSII.1
- Preoperative airway evaluation should be performed, and if there is a concern for difficult intubation, an awake induction may be considered in place of RSII.2
- Whenever RSII is performed, a backup plan for airway management must be in place in case of an unanticipated difficult intubation.2
3. Hypotension
- RSII can cause hypotension due to several factors, including the rapid administration of anesthetic medications, the induction of anesthesia itself, and the intubation procedure.2
- Frail patients and patients presenting for emergency surgery with preexisting hemodynamic instability are at high risk for hypotension.2
- In general, elderly patients are known to be chronically volume-contracted and may become hypotensive at the loss of vagal tone with RSII.2
- Hypotension during RSII can be managed with fluid resuscitation, vasoactive medications, or adjustment of anesthetic dosing.2,4
- If possible, RSII in hypotensive trauma patients or patients with compensated hemorrhagic shock should be delayed either until effective resuscitation has occurred or vasopressors have been administered. Resuscitative endovascular balloon occlusion of the aorta (REBOA) may be used as an adjunct to RSII to prevent cardiovascular collapse and secondary traumatic arrest.2,4
4. Pulmonary aspiration
- The risk for regurgitation or aspiration is present during every RSII, even when protocols are followed closely.2
- Aspiration may also occur during tracheal extubation. Before a cuffed tracheal tube is removed, it should be ensured that the patient can protect their airway prior to tube removal. Additionally, if the patient has a nasogastric tube in place, it should be suctioned prior to extubation.2
References
- Cook TM, Woodall N, Frerk C. Major complications of airway management in the United Kingdom: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011;106(5):617-31. PubMed1. Cook TM, Woodall N, Frerk C. Major complications of airway management in the United Kingdom: results of the Fourth National Audit Project of the Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth. 2011;106(5):617-31. PubMed
- Collins J, O’Sullivan EP. Rapid sequence induction and intubation. BJA Education. 2022;22(12):484-90. PubMed
- Zdravkovic M, Rice MJ, Brull SJ. The clinical use of cricoid pressure: First, do no harm. Anesth Analg. 2021;132(1):261-7. PubMed
- Park CY, Kim OH, Change SW, et al. Clinical practice guideline for airway management and emergency thoracotomy for trauma patients from the Korean Society of Traumatology. J of Trauma and Injury. 2020;33(3):195-203. Link
- Berkow LC. Rapid sequence induction and intubation (RSII) for anesthesia. Post TW, ed. UpToDate. 2022. Accessed Feb 2022. Link
- Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251-70. PubMed
- Smith KJ, Dobranowski J, Yip G, et al. Cricoid pressure displaces the esophagus: an observational study using magnetic resonance imaging. Anesthesiology. 2003;99(2):60-4. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.