Copy link
Protamine Reactions
Last updated: 01/30/2025
Key Points
- Reactions to protamine are typically classified based on clinical presentation as Type I (mild, isolated hypotension), Type II (features of anaphylactoid/anaphylactic reactions), or Type III (elevated pulmonary artery pressures, right ventricular failure).
- Independent risk factors for protamine reaction include neutral protamine hagedorn (NPH) insulin use, documented fish allergy, and a history of nonprotamine medical allergies.
- Protamine reactions are typically managed by pausing/slowing the infusion, administration of fluids and vasopressors, and for more severe reactions, with heparinization and initiation of cardiopulmonary bypass (CPB) or extracorporeal membrane oxygenation (ECMO).
Introduction
- Protamine is a positively charged, highly basic peptide that is utilized to neutralize the anticoagulant effect of negatively charged heparin through electrostatic binding. It is the only available agent in clinical use to reverse unfractionated heparin.
- Protamine has a rapid onset of action, with a heparin-neutralizing effect within 5 minutes for unfractionated heparin. Protamine only partially reverses the effects of low molecular weight heparin.
- Administration of protamine may be associated with immunological and inflammatory reactions, which include hypotension, bradycardia, pulmonary vasoconstriction, and anaphylaxis, as frequently reported clinical presentations.
- Various mechanisms have been implicated in the pathophysiology of protamine reactions. These include endothelial nitric oxide release, nonimmunologic mast cell degranulation/activation, complement activation from IgG antibodies or direct activation due to heparin-protamine complexes, and IgE and/or IgG antibody formation (Figure 1).
- The reported incidence of adverse reactions from protamine varies from 0.06% to 10.6%.1,2
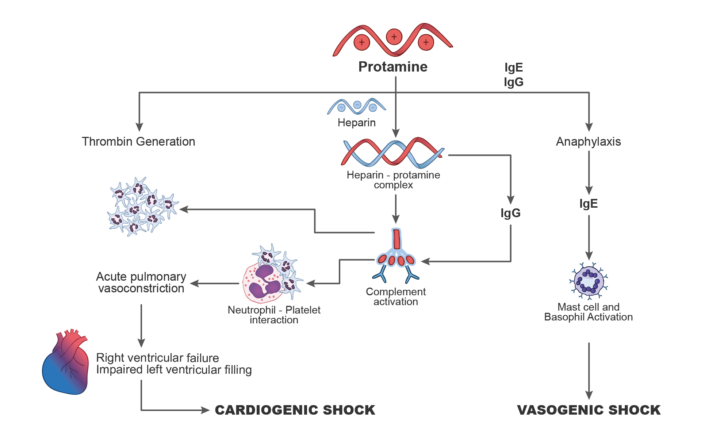
Figure 1. Mechanisms of protamine reactions. Redrawn from Levy JH, et al. What's fishy about protamine? Clinical use, adverse reactions, and potential alternatives. J Thromb Haemost. 2023;21(7):1714-23.
Risk Factors
- Risk factors for protamine reactions are listed in Table 1.
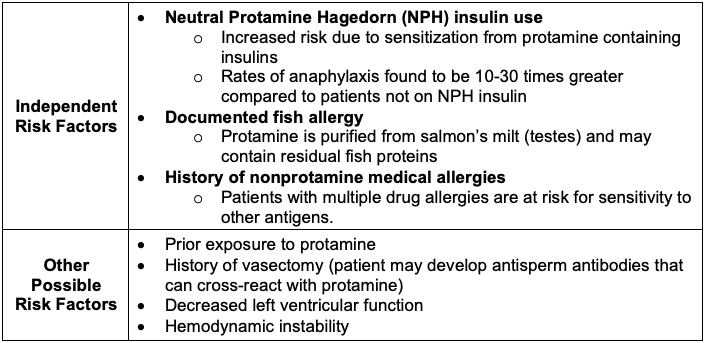
Table 1. Risk factors for protamine reactions2,3
Classification
- Mechanisms and clinical presentations of protamine reactions are listed in Table 2.
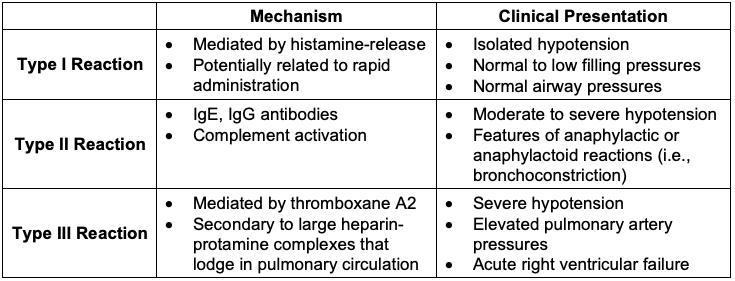
Table 2. Mechanisms and clinical presentations of protamine reactions3,4
Prevention
- Administration of a test dose (5 to 10 mg) to mitigate dose-dependent reactions
- Monitor for approximately 5 minutes following the test dose
- Protamine reactions may still occur despite a negative test dose
- Slow administration of protamine (no more than 20 mg per minute or 10-15 minutes for the entire dose)
- Close monitoring is required during administration (vital signs, transesophageal echocardiography, PA pressures, airway pressures)
- The site (central vs. peripheral) of injection has NOT been shown to influence the incidence of reaction
- Peripheral injection was previously thought to be preferred due to the increase in histamine levels associated with central injection. However, studies have not demonstrated a difference in the incidence of reactions.
- Limit the dose of protamine to less than 2.6 mg/100 units of heparin
- Typical dosing cited as approximately 1 mg/100 units of heparin.
- Higher doses are associated with inhibited platelet function, prolonged activated clotting time, increased risk of bleeding.
- In patients with prior protamine-related adverse events, consider alternatives to heparin (i.e., bivalirudin)
- Consider allowing the effect of heparin to cease over time without reversal
- This may lead to increased bleeding and increased transfusion requirements.
- Pretreatment with antihistamines has NOT been shown to be preventative.
Treatment
- Hypotension can be mitigated by slowing or pausing the protamine infusion while fluids are administered intravenously or through the aortic cannula.
- Support hemodynamics
- Vasoactive medications: phenylephrine, ephedrine, calcium chloride, norepinephrine, vasopressin
- Inotropic medications: epinephrine, milrinone
- Pulmonary vasodilators (i.e., nitric oxide, epoprostenol)
- Nebulized albuterol may be administered for the management of bronchospasm and elevated airway pressures.
- In cases of severe systemic hypotension, pulmonary hypertension, and RV failure, reheparinization and return to CPB or the initiation of venoarterial ECMO may be needed.
- There is no clear consensus regarding the reversal of anticoagulation after a protamine reaction has occurred, as some recommend slow re-dosing while others recommend cessation of protamine administration. Multidisciplinary discussions with the surgical and perfusion team are necessary for patients who have had reactions regarding the decision to reverse anticoagulation. If reversal is held, the patient will likely have a significantly increased need for blood product transfusion.
References
- Boer C, Meesters MI, Veerhoek D, Vonk ABA. Anticoagulant and side-effects of protamine in cardiac surgery: a narrative review. Br J Anaesth. 2018;120(5):914-27. PubMed
- Levy JH, Ghadimi K, Kizhakkedathu JN, Iba T. What's fishy about protamine? Clinical use, adverse reactions, and potential alternatives. J Thromb Haemost. 2023;21(7):1714-23. PubMed
- Sarwar MF, Searles BE, Stone ME, et al. Anesthesia for Cardiac Surgical Procedures. Gropper, M et al. Miller's Anesthesia. 9th ed. E-book. Pages 1731-2.
- Crivellari M et al. Protamine and heparin interactions: A narrative review. Ann Card Anaesth. 2024;27(3):202-212. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.