Copy link
Postreperfusion Syndrome
Last updated: 01/13/2025
Key Points
- Postreperfusion syndrome (PRS) poses a considerable challenge in liver transplantation, contributing significantly to morbidity and mortality for both recipients and grafts.
- PRS is a complex multiorgan process characterized by marked hypotension within five minutes of graft revascularization, often accompanied by severe electrolyte derangements, cardiac dysrhythmias, and fibrinolysis.1
- Although many observational studies have identified potential risk factors for PRS, few randomized controlled trials have been conducted to confirm these findings or evaluate innovative prevention and treatment approaches.
- Core management strategies for PRS involve volume resuscitation, vasopressor and inotropic support, correction of electrolyte disturbances, and restoration of a normal heart rhythm.
Introduction
- First described in 1987, PRS was originally described as cardiovascular collapse following liver graft reperfusion and defined as a decrease in mean arterial pressure (MAP) of more than 30% below the anhepatic phase baseline within five minutes of reperfusion of the graft, lasting at least one minute.2
- PRS has since been further subdivided into mild and severe forms:3
- Mild PRS is a MAP reduction of less than 30%, lasting under five minutes, often accompanied by bradycardia, requiring calcium or epinephrine boluses for pressure support without the need for a continuous vasopressor infusion.
- Severe PRS entails a sustained decrease in MAP exceeding 30%, associated with asystole or other cardiac dysrhythmias requiring prolonged vasopressor infusion, with or without fibrinolysis (Figure 1).
- The reported incidence of PRS ranges widely between 6-77% of patients undergoing liver transplantation, which is largely attributable to the variable definitions of PRS.1,4
Risk Factors
- Numerous prospective and retrospective studies have linked donor, recipient, and procedural factors to PRS development, though few RCTs have definitively validated these findings.4
- Donor/graft-related factors: advanced donor age, prolonged cold ischemia time, presence of macrovesicular steatosis, and size mismatch (larger graft for a smaller recipient)
- Recipient-related factors: advanced age, higher model for end-stage liver disease (MELD) scores, elevated creatinine, hyperkalemia, hypocalcemia, anemia, pre-existing left ventricular dysfunction, and fulminant hepatic failure
- Procedural factors: prolonged warm ischemia time, absence of portal vein flushing prior to reanastomosis, and use of the classical inferior vena cava (IVC) interposition technique without piggyback anastomosis
Pathophysiology4,5
- The liver typically contains 250-500 mL of blood. Upon reperfusion, cardiac preload is reduced due to the need to refill the cold donor graft. Blood passing through the graft is subsequently chilled, and some preservation fluid is flushed into the systemic circulation, resulting in myocardial depression due to the decrease in temperature and associated electrolyte disturbances.
- Furthermore, reperfusion of ischemic bowel, caused by venous congestion and surgical handling during the hepatectomy phase, leads to the release of acidic fluids, cytokines, and endotoxins that further depress myocardial function and trigger an inflammatory cascade resulting in persistent systemic vasodilation.
- Reperfusion of the ischemic graft induces cellular edema and apoptosis due to altered Na/K/ATPase function. Release of reactive oxygen species (ROS) results in the activation of Kupffer cells, which are responsible for the further release of inflammatory cytokines such as tumor necrosis factor-alpha (TNF⍺) and interleukins 1, 6, and 8 (IL-1, IL-6, and IL-8).
- Most liver graft injury during transplantation is attributed to this inflammatory response.
Management and Outcomes (Figure 1)
- Treatment of PRS aims to reverse the pathologic derangements described above:
- Fluid resuscitation is crucial to maintain cardiac output following the 250-500mL decrease in preload during graft reperfusion.
- Heart rate stabilization is necessary to optimize cardiac output. Severe bradycardia and tachycardia must be promptly managed, and arrhythmias corrected to restore sinus rhythm.
- Vasopressors are employed to combat the vasodilatory effect of inflammatory cytokines released by the liver and bowel during reperfusion of ischemic tissue.
- Inotropes are often required to address myocardial depression caused by the influx of cold preservation solution along with inflammatory mediators released from the ischemic liver graft.
- Electrolyte and acid-base correction typically involve calcium and magnesium supplementation (both reduced by citrate chelation during blood product transfusion), bicarbonate administration, and management of serum potassium reduction.
- Investigative therapies used for the treatment of refractory PRS include methylene blue (a scavenger of reactive oxygen species-ROS), hydroxocobalamin (a scavenger of nitric oxide-NO), acetylcysteine (an antioxidant via restoration of glutathione stores), protease inhibitors (to reduce fibrinolysis), and magnesium sulfate (to suppress inflammatory cytokine production).5
- Patients with severe PRS have been shown to require more blood product (red blood cells, fresh-frozen plasma, and cryoprecipitate) transfusions than those with mild or no PRS.3,6
- Severe PRS is also associated with higher rates of postoperative renal dysfunction, extended ventilatory support, prolonged ICU and hospital stays, and a greater need for retransplantation.3,6
- Determining the precise impact of PRS on patient and graft survival is challenging due to confounding variables related to recipient, graft, and procedural factors.
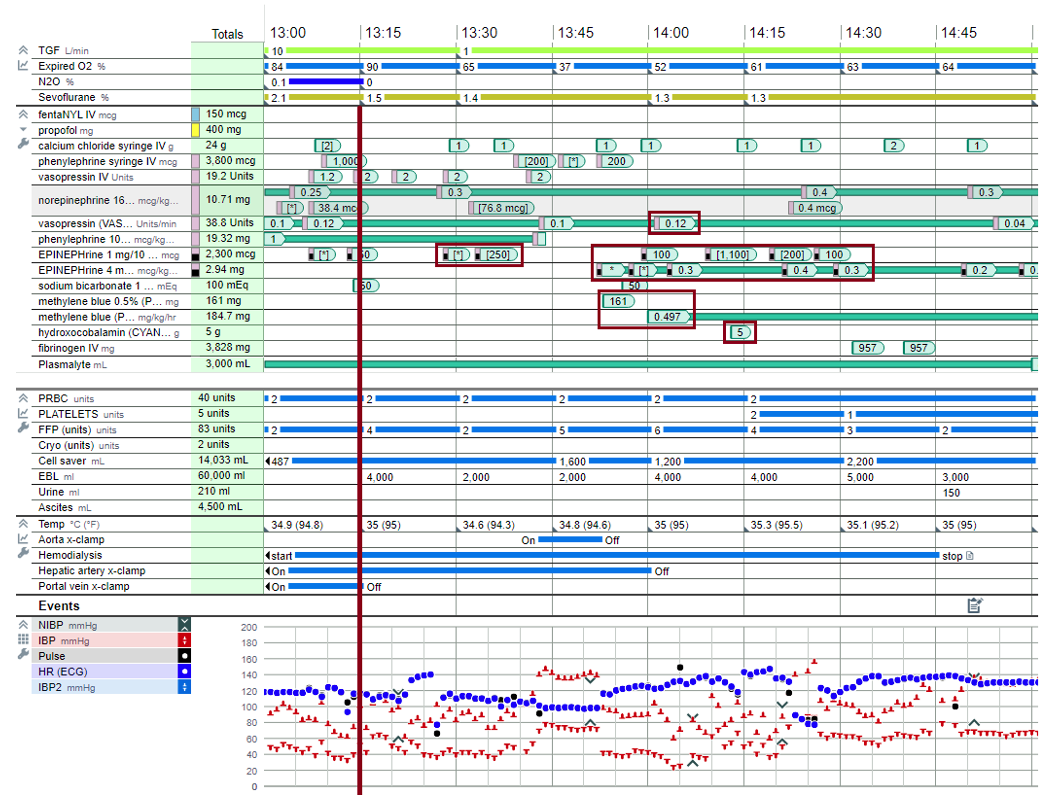
Figure 1. The intraoperative anesthesia record of a patient experiencing severe PRS requiring a significant increase in pressor support, blood product transfusion, and ultimately the administration of methylene blue and hydroxocobalamin. The vertical red line represents the time of graft reperfusion. Note the background infusions of vasopressin, norepinephrine, and phenylephrine at the time of reperfusion and the clamping of the aorta.
References
- Fukazawa K, Pretto Jr EA. The post-reperfusion syndrome (PRS): diagnosis, incidence and management. In: Abdeldayem H, Allam N (Eds.). Liver Transplantation - Basic Issues. IntechOpen; 2012: 385-96. Link
- Aggarwal S, Kang Y, Freeman JA, et al. Postreperfusion syndrome: cardiovascular collapse following hepatic reperfusion during liver transplantation. Transplant Proc. 1987;19(4 Suppl 3):54-5. PubMed
- Hilmi I, Horton CN, Planinsic RM et al. The impact of postreperfusion syndrome on short-term patient and liver allograft outcome in patients undergoing orthotopic liver transplantation. Liver Transpl. 2008;14(4):504-8. PubMed
- Siniscalchi A, Gamberini L, Laici C et al. Post reperfusion syndrome during liver transplantation: from pathophysiology to therapy and preventive strategies. World J Gastroenterol. 2016;22(4):1551-69. PubMed
- Manning MW, Kumar PA, Maheshwari K et al. Post-reperfusion syndrome in liver transplantation-an overview. J Cardiothorac Vasc Anesth. 2020;34(2):501-11. PubMed
- Paugam-Burtz C, Kavafyan J, Merckx P et al. Postreperfusion syndrome during liver transplantation for cirrhosis: outcome and predictors. Liver Transpl. 2009;15(5):522-9. PubMed
Other References
- Wagener G. Liver transplantation: Anesthetic management. In: UpToDate. 2024. Accessed 1/6/2025 Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.