Copy link
Postoperative Nausea and Vomiting in Children
Last updated: 03/08/2023
Key Points
- Postoperative nausea and vomiting (PONV), although not life-threatening, is the most common complication following general anesthesia in pediatric patients.
- The risk of PONV is twice as high in children than in adults.
- There is an increased risk of PONV with strabismus surgery, adenotonsillectomy, otoplasty, and surgeries lasting longer than 30 minutes.
- PONV prophylaxis should be given based on a risk stratification of patients. A multimodal approach should be used to prevent and treat PONV in children.
Introduction
- PONV is the most common complication following general anesthesia in pediatric patients.
- Although not life-threatening, PONV is uncomfortable for the patient and can lead to worsened patient and family dissatisfaction.
- The incidence of PONV in children is estimated to range from 33 to 82%.1,2 Since small children and patients with developmental delay cannot verbally report feeling nauseous, postoperative vomiting is more commonly measured in research studies.
- Uncontrolled PONV can lead to an increased length of stay in the postanesthesia care unit or an unanticipated hospital admission after outpatient surgery. Other complications include possible wound dehiscence, dehydration, and pulmonary aspiration.2
Risk Factors
- Risk factors for PONV can be categorized as surgical, anesthetic, or patient-related.
- Surgical risk factors:3
- strabismus surgery;
- adenotonsillectomy;
- otoplasty;
- intraabdominal surgeries (especially laparoscopic); and
- surgery lasting longer than 30 minutes.
- Anesthetic risk factors:3
- use of volatile anesthetics;
- administration of anticholinesterases (i.e., neostigmine); and
- administration of long-acting opioids.
- Patient-related risk factors:3
- age 3 years and older;
- previous history of PONV or motion sickness;
- family history of PONV; and
- postpubertal female.
Prevention and Treatment of PONV
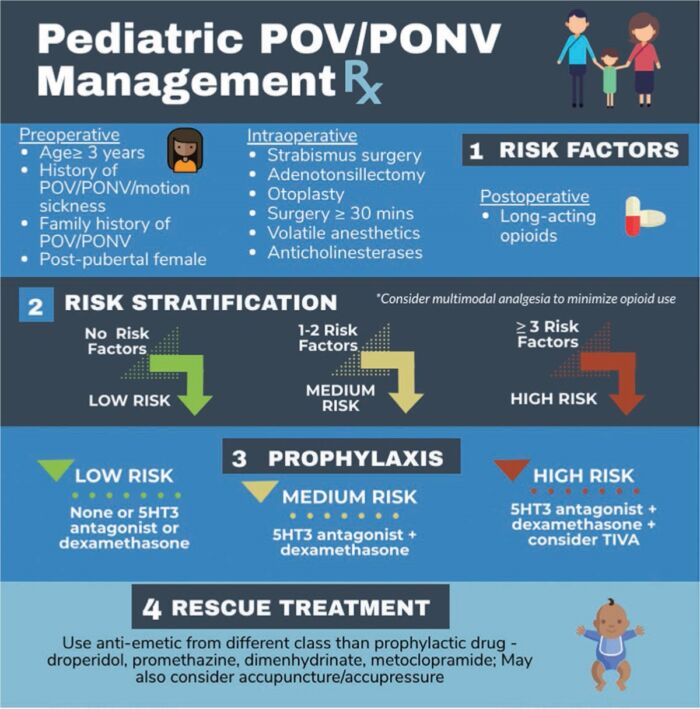
Figure 1. Algorithm for the management of PONV in children. Reproduced with permission from the American Society for Enhanced Recovery.
Pharmacologic Prophylaxis
- 5-HT3 Receptor Antagonists (Ondansetron)
- Ondansetron (0.1-0.15 mg/kg up to 4 mg) is the most used antiemetic and is considered the “gold standard” in PONV management. Ondansetron has the strongest evidence of all antiemetics in children.2,3
- There is a potential risk of dose-dependent QT prolongation resulting in ventricular arrhythmias, especially torsades de pointes. Ondansetron should be avoided in children with congenital long QT syndromes.2
- Ondansetron has a half-life of approximately 4 hours which is why it is often administered at the end of the anesthetic. However, a recent Cochrane review did not show any evidence to support this approach.2
- Corticosteroids (Dexamethasone)
- The mechanism of action of corticosteroids as an antiemetic is not fully understood. Central anti-inflammatory effects have been hypothesized.
- As an added benefit, corticosteroids have been shown to reduce the need for analgesics when used for antiemetic prophylaxis.2,3
- For maximum efficacy, corticosteroids should be given at the beginning of the anesthetic.2
- Dexamethasone should be used with caution in patients with newly diagnosed malignancies as it can cause tumor lysis syndrome, and it may also interfere with chemotherapy regimens.
- It may also cause hyperglycemia and therefore, should be used with caution in patients with diabetes.
- Notably, the efficacy of ondansetron in children is increased when it is used in conjunction with dexamethasone.2
- Antimuscarinics (Scopolamine)
- Transdermal scopolamine is not currently FDA approved for use in children younger than 12 years. However, it can be used in high-risk adolescent patients.
- The transdermal patch should be applied before the induction of general anesthesia.
- Side effects include dry mouth, dizziness, and blurred vision.
- Antidopaminergics (Droperidol)
- Droperidol (0.05-0.75 mg/kg, up to a maximum dose of 1.25 mg) is an effective antiemetic. In 2001, the FDA issued a black box warning on the use of droperidol secondary to the risk of QT prolongation and ventricular arrhythmias. Despite this FDA warning being challenged by many anesthesiologists, droperidol use for PONV has fallen out of favor.3
- Droperidol is most effective when administered at the end of the case.
- Antidopaminergics also have the potential for extrapyramidal side effects such as akathisia, dystonia, tardive dyskinesia, and Parkinsonism.
- Neurokinin-1 Receptor Antagonists (Aprepitant)
- Aprepitant is a neurokinin-1 (NK-1) receptor antagonist that is FDA approved for chemotherapy-induced nausea and vomiting in children older than 6 months.
- Aprepitant has a half-life of 40 hours, so its use as an antiemetic may have a role in longer term control of PONV.
- Antihistamines (Diphenhydramine, Dimenhydrinate)
- Antihistamines treat PONV by inhibiting acetylcholine and histamine receptors in the nucleus tractus solitarius and vestibular systems.
- They may cause oversedation.
- Propofol
- Multiple systematic reviews support the use of propofol total intravenous anesthetic (TIVA) as an effective intervention in reducing the risk for PONV in children undergoing strabismus surgery.3-5 However, TIVA has been reported to increase the rate of oculocardiac reflex during strabismus surgery in children.
- Prokinetics (Metoclopramide)
- The use of metoclopramide has been discouraged in children due to the higher risk of extrapyramidal symptoms, including about a 20 times higher risk of dyskinesias in children compared to adults.2
Nonpharmacologic Prevention Strategies
- When possible, heavy opioid use should be minimized. Regional anesthesia should be considered to reduce opioid requirements.
- Excessive fasting should be minimized as it has been linked to an increased incidence of PONV.6
- Liberal intravenous fluid resuscitation up to 30 mL/kg has been shown to reduce PONV in pediatric patients undergoing same-day surgery.7
- In high-risk patients, avoiding volatile anesthetics by utilizing TIVA should be considered.
Rescue Therapy
- Rescue antiemetic treatment should be from a different pharmacological class than the prophylactic treatment. Administering an additional dose of antiemetic from the same class within 6 hours of the initial dose does not have any therapeutic benefit.
- Other therapies include nonpharmacological options, including distraction (tablet, television, music), aromatherapy, or acupuncture.
- There is literature to support the use of isopropyl alcohol as aromatherapy. In these studies, alcohol swabs or gauze saturated with isopropyl alcohol was placed underneath the patient’s nose to inhale. Isopropyl alcohol was shown to reduce the duration and severity of nausea compared to placebo and conventional pharmacotherapy. Of note, it was shown to be ineffective for prophylaxis.8
- A Cochrane review demonstrated that acupuncture can potentially reduce the incidence of PONV; however, when compared to the use of antiemetic drugs as prophylaxis, there was no difference.9
- It is also essential to search and treat for reversible causes of PONV, including excessive opioids, mechanical bowel obstruction, and blood in the pharynx and stomach.
References
- Eberhart LH, Morin AM, Guber D, et al. Applicability of risk scores for postoperative nausea and vomiting in adults to paediatric patients. Br J Anaesth. 2004;93(3):386-92. PubMed
- Ames WA, Machovec K. An update on the management of PONV in a pediatric patient. Best Pract Res Clin Anaesthesiol. 2020;34(4):749-58. PubMed
- Gan TJ, Belani KG, Bergese S, et al. Fourth consensus guidelines for the management of postoperative nausea and vomiting. Anesth Analg. 2020;131(2):411-48. PubMed
- Schaefer MS, Kranke P, Weibel S, et al. Total intravenous anesthesia vs single pharmacological prophylaxis to prevent postoperative vomiting in children: A systematic review and meta-analysis. Paediatr Anaesth. 2017;27(12):1202-9. PubMed
- Scheiermann P, Herzog F, Siebenhofer A, et al. Intravenous versus inhalational anesthesia for pediatric inpatient surgery - A systematic review and meta-analysis. J Clin Anesth. 2018;49:19-25. PubMed
- Fawcett WJ, Thomas M. Pre-operative fasting in adults and children: clinical practice and guidelines. Anaesthesia. 2019;74(1):83-8. PubMed
- Ashok V, Bala I, Bharti N, et al. Effects of intraoperative liberal fluid therapy on postoperative nausea and vomiting in children-A randomized controlled trial. Paediatr Anaesth. 2017;27(8):810-5. PubMed
- Hines S, Steels E, Chang A, et al. Aromatherapy for treatment of postoperative nausea and vomiting. Cochrane Database Syst Rev. 2018;3(3):CD007598. PubMed
- Lee A, Chan SK, Fan LT. Stimulation of the wrist acupuncture point PC6 for preventing postoperative nausea and vomiting. Cochrane Database Syst Rev. 2015;(11):CD003281. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.