Copy link
Polysomnography for Anesthesiologists
Last updated: 09/10/2024
Key Points
- Obstructive sleep apnea (OSA) is a common type of sleep-disordered breathing (SDB) encountered in clinical practice that requires careful planning in the perioperative period.1 Between 60-90% of OSA patients remain undiagnosed in the perioperative setting.1
- There has been a recent increase in the percentage of ambulatory and daycare surgical procedures, including patients with OSA. The perioperative outcome of such patients depends on the diagnosis and management of the condition, although the suitability of OSA patients posted for ambulatory surgeries remains controversial.
- OSA is associated with an increased risk of perioperative morbidity and mortality. Still, the perioperative diagnosis of such cases is complicated by poor recognition, understanding, and utilization of available diagnostic tools such as polysomnography (PSG).2
- A proper understanding of PSG helps in the appropriate perioperative management of OSA patients.3
Definitions
• SDB refers to a spectrum of sleep-related conditions, including increased upper airway resistance to airflow, heavy snoring, marked reduction in airflow (hypopnea), and complete cessation of breathing (apnea). Increased resistance to airflow without apnea is classified as upper airway resistance syndrome. Apneas and hypopneas are further classified as central, obstructive, or mixed.
• The most common type of SDB is OSA, which is characterized by episodes of complete or partial collapse of the upper airways with an associated decrease in oxygen saturation or cortical arousal from sleep.2
• A PSG is the gold standard for diagnosing SDB.2 It is a laboratory-based sleep study that diagnoses and allows for further risk stratification of SDB.
Indications
• Common indications for PSG are listed in Table 1.
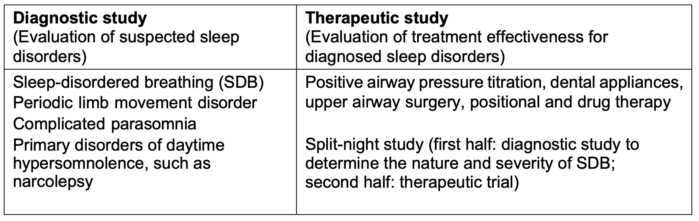
Table 1. Indications for polysomnography
Types of Monitors
- According to the American Academy of Sleep Medicine (AASM), sleep study monitors can be categorized into four types based on the complexity of monitoring and the type of monitors used.2
- The types of monitors used for evaluating sleep disorders are listed in Table 2.
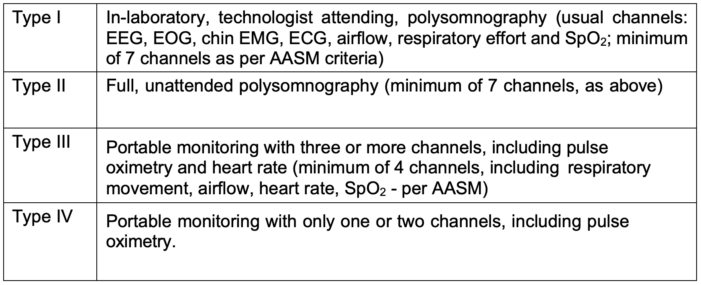
Table 2. Types of sleep study monitors. Abbreviations: AASM = American Academy of Sleep Medicine; EEG = electroencephalography; ECG = electrocardiography; EMG = electromyography; EOG = electrooculography; PSG = polysomnography; SpO2 = oxygen saturation
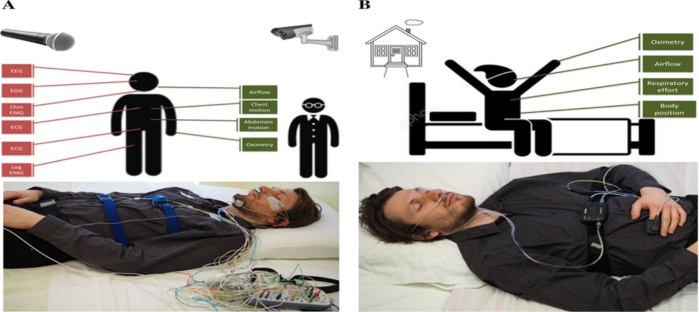
Figure 1. Differences between laboratory-based (type I) and portable PSG. A: In a laboratory-based PSG, various electrodes are applied to monitor EEG, EOG, chin EMG, ECG, airflow, respiratory effort, and oxygen saturation. A video camera in the room records body position and parasomnia behavior. A microphone is used to record snoring. A registered sleep technologist is present to set up, monitor, and verify the accuracy of the recording. B: Home sleep study with a type III monitor. The study is conducted in the comfort of the patient’s home. A minimum of four channels are used to record respiratory effort, airflow, heart rate, and oxygen saturation. Used with permission from Meliana V et al. Interpretation of sleep studies for patients with sleep-disordered breathing: What the anesthesiologist needs to know. Can J Anaesth. 2018;65(1):60-75. PubMed
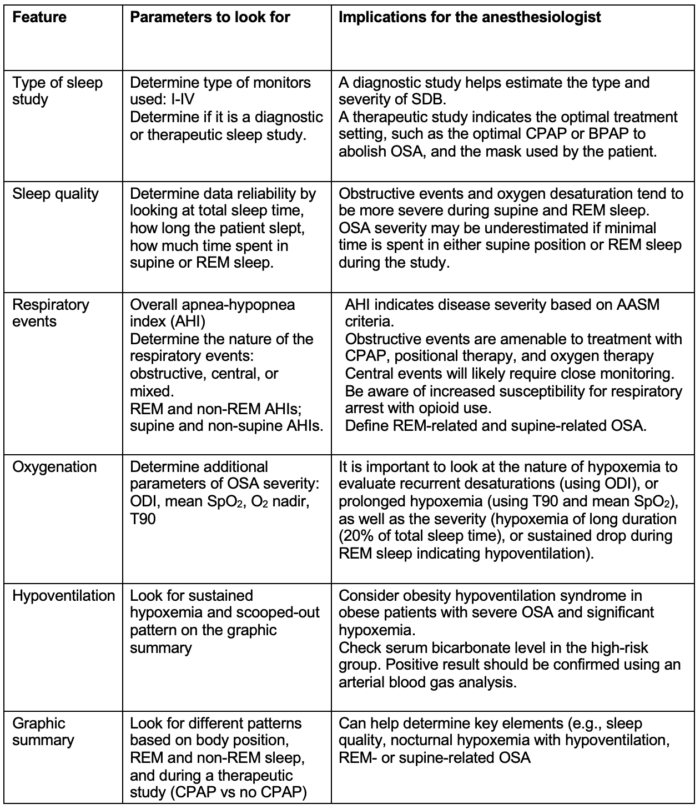
Table 3. Interpretation of a polysomnography. Abbreviations: AASM = American Academy of Sleep Medicine; AHI = apnea-hypopnea index; BPAP = bi-level positive airway pressure; CPAP = continuous positive airway pressure; ODI = oxygen desaturation index; OSA = obstructive sleep apnea; PSG = polysomnography; REM = rapid eye movement; T90 = percentage of total sleep time spent with SpO2 < 90%.
OSA and Perioperative Complications
- Undiagnosed OSA patients are at three times higher risk of perioperative cardiac events as compared to diagnosed patients managed with preoperative continuous positive airway pressure (CPAP) therapy.
- There is a strong correlation between OSA severity and the risk of nocturnal sudden cardiac death. Patients with severe OSA (AHI ≥ 40) had a 40% rise in relative risk for sudden cardiac death compared to those with mild to moderate OSA (AHI 5-39).2
- Common cardiac events include atrial and ventricular arrhythmias, myocardial infarction, nocturnal sudden cardiac death, heart failure, and embolism.
- Postoperative respiratory complications are about three times higher in patients with AHI greater than 30.4
- Common respiratory complications include respiratory failure, emergent intubation, non-invasive or mechanical ventilation, and pneumonia.
- AHI typically increases on the first night, with a peak increase on the third night.
- Patient’s age, preoperative AHI, and opioid dosage are significant predictors of postoperative AHI.
References
- Singh M, Liao P, Kobah S, et al. Proportion of surgical patients with undiagnosed obstructive sleep apnoea. Br J Anaesth. 2013;110(4):629-36. PubMed
- Meliana V, Chung F, Li CK, Singh M. Interpretation of sleep studies for patients with sleep-disordered breathing: What the anesthesiologist needs to know. Can J Anaesth. 2018;65(1):60-75. PubMed
- Sankar A, Dixon PR, Sivanathan L, et al. Cost-effectiveness analysis of preoperative screening strategies for obstructive sleep apnea among patients undergoing elective inpatient surgery. Anesthesiology. 2020;133(4):787-800. PubMed
- Mutter TC, Chateau D, Moffatt M, et al. A matched cohort study of postoperative outcomes in obstructive sleep apnea: could preoperative diagnosis and treatment prevent complications? Anesthesiology. 2014;121(4):707-18. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.