Copy link
Platelets
Last updated: 12/19/2024
Key Points
- Platelets are one of the necessary components required for initial hemostasis and can be transfused to aid in the cessation of bleeding.
- A therapeutic platelet transfusion should be considered for the patient with ongoing bleeding in the setting of thrombocytopenia or platelet dysfunction. Prophylactic platelet transfusions have been recommended in various situations for the prevention of spontaneous bleeding or anticipation of an invasive procedure.
- The standard adult dose is one apheresis unit or six units of whole blood-derived platelets, which is expected to increase the platelet count by 30-60 x 109/L.
Introduction
- Platelets are necessary for primary hemostasis and contribute to forming the hemostatic plug. Platelet adhesion occurs at the site of injury, activating and aggregating the platelets. This eventually leads to clot formation through the coagulation cascade.1
- While a platelet count between 150 and 450 x 109/L is considered normal, a sufficient count may not translate to adequate primary hemostasis due to platelet function disorders or the use of antiplatelet medications.
- Platelet transfusion indications can be broadly divided into therapeutic and prophylactic. Various medical societies provide guidelines on the appropriate use of platelet transfusions. While some of these recommendations lack robust evidence, following the published guidelines can help reduce the risks associated with platelet transfusions.
Platelet Preparations
- Platelets are collected either by apheresis from a single donor or separation from whole blood collections. Whole blood-derived platelets are generally pooled, with six units approximating one unit of apheresis platelets (≥ 3.0 x 1011 platelets).1
- Platelet components contain varying levels of leukocytes and red blood cells depending on the collection method.1
- Platelets are suspended in plasma or a platelet additive solution containing various substances, including citrate and dextrose. The storage bags allow for oxygen and carbon dioxide exchange.2
- Platelets usually have a shelf life of 5-7 days, depending on the preparation and collection method.1
- Platelets are generally stored at room temperature (20-24°C), but some studies have investigated cold storage (2-6°C), which could increase shelf life and decrease bacterial contamination.3
- Leukoreduction is a filtration process that decreases the number of leukocytes in platelet components. It is standard practice in many centers and can reduce the risk of HLA alloimmunization, cytomegalovirus transmission, and febrile nonhemolytic transfusion reactions.1
- Platelets can be irradiated to inhibit the proliferation of T lymphocytes, thus preventing transfusion-associated graft-versus-host disease. Irradiated platelets should be used for patients in specific immunocompromised states, including neonates, stem-cell transplant recipients, patients taking purine analogs, and those with particular hematological malignancies, Hodgkin lymphoma, or congenital immunodeficiencies. Platelets should also be irradiated if the donor is a blood relative to the recipient.1
- Please see the OA summary on blood product modifications for more details. Link
Clinical Uses
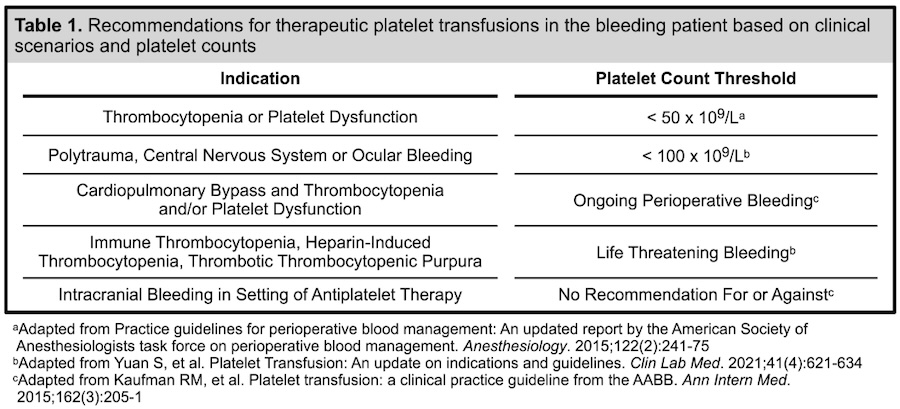
Therapeutic Platelet Transfusions
- Per the 2015 American Society of Anesthesiologists Practice Guidelines for Perioperative Blood Management, platelet transfusions may be indicated for the bleeding patient in the setting of thrombocytopenia (platelets less than 50 x 109/L) or platelet dysfunction. It is recommended that a platelet count be obtained prior to transfusion, and a test of platelet function should be performed if platelet dysfunction is suspected.4
- Platelet counts should be maintained above 100 x 109/L in patients with ongoing bleeding in the setting of polytrauma, central nervous system bleeding, or ocular bleeding.5
- Massive transfusion protocols generally suggest transfusion of red blood cells, fresh frozen plasma, and platelets in a 1:1:1 ratio, keeping in mind that one apheresis unit of platelets is equivalent to 6 units of whole blood-derived platelets.
- A platelet transfusion may be indicated for patients undergoing cardiopulmonary bypass if there is clinical bleeding in the setting of thrombocytopenia or platelet dysfunction.6
- The Association for the Advancement of Blood and Biotherapies (AABB) cannot recommend for or against platelet transfusions for patients with intracranial bleeding in the setting of antiplatelet therapy, and specific patient factors should be considered before the transfusion of platelets.6
- Platelet transfusions are contraindicated in patients with thrombotic thrombocytopenic purpura or heparin-induced thrombocytopenia unless the patient has life-threatening bleeding due to an increased risk of arterial thrombosis.5
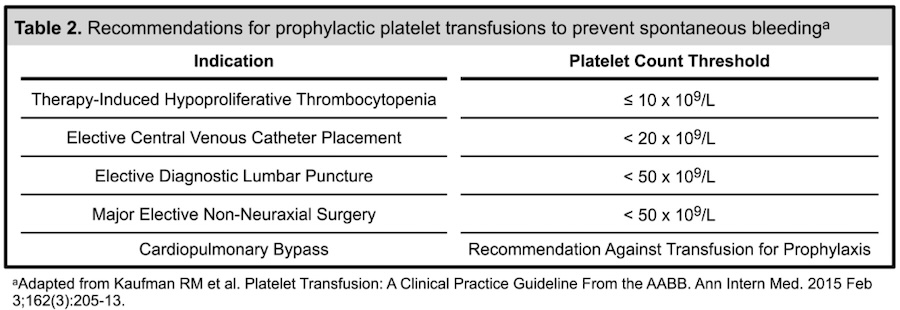
Prophylactic Platelet Transfusions
- The 2015 Clinical Practice Guideline from the AABB6 recommends a prophylactic platelet transfusion for patients as follows:
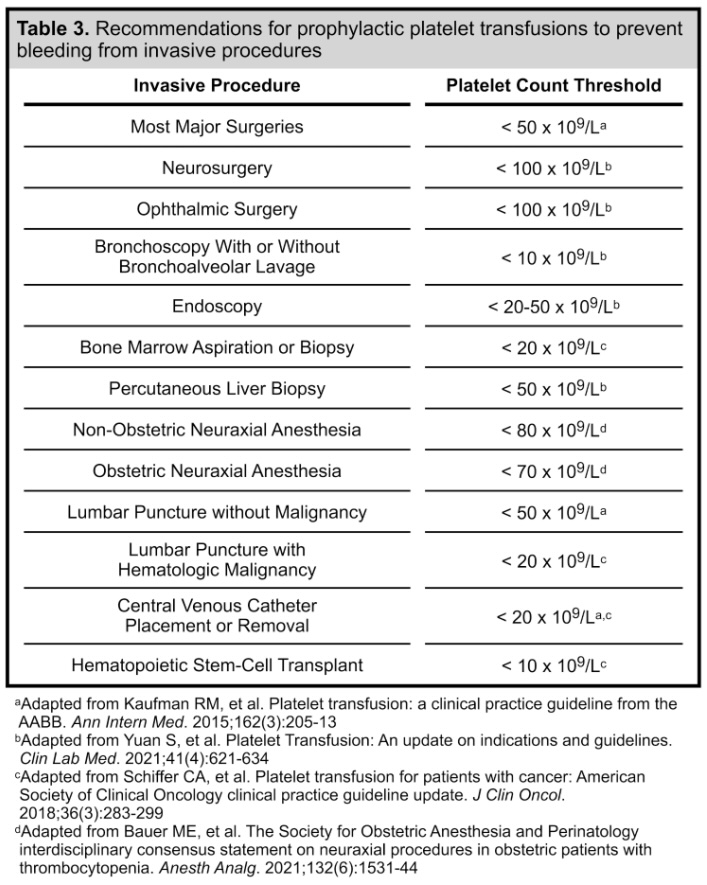
- Prophylactic platelet transfusions may also be indicated prior to neurosurgery or ophthalmic surgery (< 100 x 109/L), bronchoscopy (< 10 x 109/L), endoscopic procedures (< 20-50 x 109/L), percutaneous liver biopsies (< 50 x 109/L),5 or bone marrow aspiration and biopsies (< 20 x 109/L).7
- Platelet transfusions should be considered for patients with thrombocytopenia (< 20 x 109/L) and hematologic malignancies undergoing lumbar puncture.7
- Platelets should be at least 70 x 109/L prior to obstetric neuraxial anesthesia or 80 x 109/L prior to nonobstetric neuraxial anesthesia. Still, no recommendations exist to transfuse platelets if levels fall below these values.8
- Patients with hematologic or solid organ malignancies receiving therapy and patients undergoing allogenic hematopoietic stem-cell transplant should be transfused for platelet counts < 10 x 109/L.7
- Platelets should be transfused for levels < 20 x 109/L to prevent bleeding in the stable neonate. Platelets should be transfused if values are < 50 x 109/L in the setting of extreme prematurity or clinical illness.9
Administration
- The standard dose of platelets for an adult patient is one apheresis platelet unit (or equivalent), which should increase the platelet count by 30-60 x 109/L.1 A dose of 5-10 mL/kg is standard for a pediatric patient. The lifespan of transfused platelets is 3-4 days, compared to the normal 8-10 days.
- Platelets should be transfused through a platelet administration set, which includes a 170–200-micron filter. Platelets should not be given in the same administration set as blood.
- Platelets are generally administered over 30 minutes, and it is recommended to complete the transfusion within 4 hours.
- While ABO-identical platelets should be the first choice, their short shelf life, and limited stock may sometimes make this impossible. Using ABO-identical platelets for transfusion may increase posttransfusion platelet counts and decrease febrile and allergic reactions, but incompatibility does not necessarily preclude their use. Patient-specific factors should be taken into account before administering incompatible platelets.10
Complications
Bacterial Contamination
- Platelets are the most common blood product to be contaminated with bacteria; the most common contaminants are gram-positive skin flora.1
- Symptoms due to the bacterial contamination of transfused platelets include fevers, chills, hypotension, or circulatory collapse that can occur immediately or several hours after transfusion.1
- Treatment is supportive and includes antibiotic therapy.
- The Food and Drug Administration has established regulations and released guidance to minimize bacterial contamination of platelet products.
- Please see the OA summary on blood transfusion complications for more details. Link
Platelet Alloimmunization
- Platelets express various surface antigens, including Class I HLA and platelet-specific antigens. Recipients of platelet transfusions can develop antibodies to these antigens, leading to a severely decreased lifespan of the transfused platelets and possible refractoriness to further transfusions.1
- When platelet refractoriness is suspected, immune-mediated causes should be differentiated from nonimmune-mediated causes, such as splenomegaly, sepsis, disseminated intravascular coagulation, intravascular devices, or medications.5
- Platelet alloimmunization is prevented by reducing unnecessary platelet transfusions and the leukoreduction of platelet components.2
- Management includes administering platelets that are HLA-matched, HLA antigen-negative, or cross-matched. This requires irradiating the unit to reduce the risk of transfusion-associated graft-versus-host disease.7
RhD Alloimmunization
- Platelet components may contain red blood cells and whole blood-derived platelets generally contain more red blood cells than apheresis platelets.1
- Although platelets do not express RhD antigens, the red blood cells that contaminate the platelet components put patients at risk of RhD alloimmunization.
- Blood donors are screened for antibodies against RhD antigens, minimizing the risk of hemolysis in RhD-positive recipients.10
- RhD-negative recipients of platelets from RhD-positive donors are at risk of forming antibodies to donor red blood cell RhD antigens (RhD alloimmunization). Administration of anti-D immune globulin should be considered depending on patient factors.10
Hemolysis
- Platelet components are suspended in plasma which can contain ABO antibodies. Although rare, transfusion of ABO-incompatible plasma could lead to hemolysis of recipient red blood cells.
- Prevention includes transfusion of only ABO identical platelets, limiting the total amount of incompatible plasma, suspending in platelet additive solution to decrease the plasma volume, testing to identify high titer units, washing, or volume reduction.10
- Please see the OA summary on blood transfusion reactions for more details. Link
Transfusion Reactions
- Transfusion reactions, including transfusion-related acute lung injury, transfusion-associated circulatory overload, febrile nonhemolytic reactions, transfusion-associated graft-versus-host disease, allergic reactions, anaphylactic reactions, and posttransfusion purpura can complicate platelet transfusions.1
- Please see the OA summary on blood transfusion reactions for more details. Link
References
- Association for the Advancement of Blood & Biogherapies ARC, America’s Blood Centers, Armed Services Blood Program. Circular of Information for the Use of Human Blood and Blood Components. Plasma Components 2021: 19-27. Link
- McCullough J. Overview of platelet transfusion. Semin Hematol. 2010;47(3):235-42. PubMed
- Strandenes G, Sivertsen J, Bjerkvig CK, et al. A pilot trial of platelets stored cold versus at room temperature for complex cardiothoracic surgery. Anesthesiology. 2020;133(6):1173-83. PubMed
- Practice guidelines for perioperative blood management: An updated report by the American Society of Anesthesiologists task force on perioperative blood management. Anesthesiology. 2015;122(2):241-75. PubMed
- Yuan S, Otrock ZK. Platelet Transfusion: An update on indications and guidelines. Clin Lab Med. 2021;41(4):621-634. PubMed
- Kaufman RM, Djulbegovic B, Gernsheimer T, et al. Platelet transfusion: a clinical practice guideline from the AABB. Ann Intern Med. 2015;162(3):205-13. PubMed
- Schiffer CA, Bohlke K, Delaney M, et al. Platelet transfusion for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2018;36(3):283-299. PubMed
- Bauer ME, Arendt K, Beilin Y, et al. The Society for Obstetric Anesthesia and Perinatology interdisciplinary consensus statement on neuraxial procedures in obstetric patients with thrombocytopenia. Anesth Analg. 2021;132(6):1531-44. PubMed
- Christensen RD, Carroll PD, Josephson CD. Evidence-based advances in transfusion practice in neonatal intensive care units. Neonatology. 2014;106(3):245-53. PubMed
- Dunbar NM. Does ABO and RhD matching matter for platelet transfusion? Hematology. 2020;2020(1):512-7. PubMed
Other References
- Klucsarits S. Platelets: How many do we need? OA-SOAP Fellows Webinar Series. 2021. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.