Copy link
Perioperative Management of Total Parenteral Nutrition
Last updated: 07/16/2025
Key Points
- Total parenteral nutrition (TPN) is a mixture of macronutrients and micronutrients administered intravenously in patients unable to receive enteral nutrition (EN) for extended periods of time.
- TPN must be administered through a central venous catheter.
- Complications associated with TPN involve those related to central venous access and metabolic derangements.
- Intraoperative glucose monitoring is highly recommended in patients receiving TPN.
Introduction
- TPN is the intravenous administration of a comprehensive nutrient solution to a patient whose gastrointestinal tract cannot be accessed or is nonfunctional. TPN is designed to provide the required macronutrients (carbohydrates, proteins, and fatty acids) and micronutrients (vitamins, electrolytes, and necessary trace elements), along with free water, to meet the patient’s metabolic requirements.1
- Due to the hyperosmolarity of the solution, TPN typically needs to be delivered via a central venous catheter. Prolonged dependence on TPN has associated risks such as catheter-related infections, thrombosis, and metabolic disturbances (hypertriglyceridemia, electrolyte imbalances, hyperglycemia, etc.). It should only be initiated when indicated and discontinued as soon as an alternative route is possible.1
Goals of Nutritional Support
- Nutritional support, especially in the perioperative setting, has gained increasing attention as an aspect of patient optimization and enhanced recovery pathway. Additionally, surgical stress increases the risk of placing patients into a hypermetabolic state. This is compounded by the problem that critically ill or chronically ill patients are more likely to be nutritionally deficient.
- Poor nutritional status has been shown to be associated with increased risk of postoperative complications. Malnourished patients experience a higher rate of wound infections, decreased wound healing, and a longer length of stay. These challenges highlight the importance of nutrition for surgical patients in the perioperative setting.2
- The goal of nutritional support is to provide the patient with baseline metabolic needs. The American Gastroenterological Association recommends caloric provision of 25 to 30 kcal/kg/day, protein at 1.0 to 1.5 g/kg/day, and lipids providing 20 to 30% of total calories for adults. This requires careful monitoring and adjustment depending on the individual needs of the patient, their clinical status and associated comorbidities, and their metabolic response.3,4
Enteral vs. Parenteral Support
- EN is the preferred route of nutritional support for hospitalized patients who have a functioning gastrointestinal tract. If they are unable to maintain oral intake, EN may be provided via nasogastric, nasojejunal, gastrostomy, or jejunostomy tubes, depending on various patient factors.
- The gut serves as an important function in providing immunity. Gut-associated lymphoid tissue is found in the gastrointestinal tract and provides 60% to 70% of innate and adaptive immunity. Additionally, the gut provides a physical barrier from infection via the presence of tight junctions between villi and the secretion of mucin. Animal studies have demonstrated loss of gastrointestinal mucosal architecture in animals who received TPN. Lack of EN causes villous blunting and increased mucosal permeability, which can increase bacterial inoculation through the gut. Consequently, the American College of Gastroenterology recommends prompt initiation of EN for patients to preserve gut integrity and prevent metabolic complications.3
- Contraindications of EN would be bowel obstruction, high flow gastrointestinal fistulas, severe hemodynamic instability requiring vasopressor support, and severe gastrointestinal bleeding.5
- Parenteral nutrition (PN) is indicated when EN is insufficient or not feasible, either due to severe malabsorption or due to a nonfunctional gastrointestinal tract. TPN is administered via a central venous catheter. In critically ill patients, studies have shown that mortality does not differ significantly between EN and PN, but EN may reduce the risk of sepsis.6
- TPN is generally contraindicated in patients when gastrointestinal feeding is possible, where fasting is expected to be less than 5 days, in terminally ill patients where death is imminent, and in patients with severe cardiovascular or metabolic instability (should be corrected prior to TPN initiation).6
TPN Components
- TPN exists as an admixture of 3 major macronutrients, micronutrients, and free water to meet the patient’s metabolic needs.7
- The three major macronutrients are carbohydrates, fats, and proteins (Table 1). Typical micronutrients include vitamins, electrolytes, minerals, and trace elements (Table 2).7,8
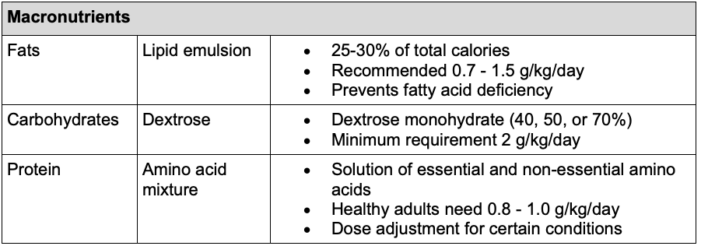
Table 1. Summary of macronutrients in TPN and recommendations according to the ESPEN guidelines9
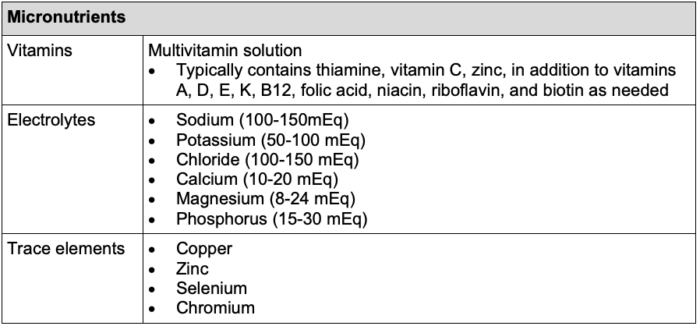
Table 2. Summary of micronutrients commonly included in TPN and recommendations according to the ESPEN guidelines9
- The composition of TPN is adjusted to fulfill the needs of each individual patient. This is especially true for protein supplementation. According to the patient’s condition, the following dosing is recommended:7
- Critically ill patients without hepatic or renal dysfunction: 1.5 g/kg/day
- Renal failure: 0.6 – 0.8 g/kg/day
- Acute hepatic encephalopathy: 0.8 g/kg/day (temporary restriction)
- Hemodialysis: 1.2 – 1.3 g/kg/day
- Continuous renal replacement (CRRT, CVVHD, CVVHDF): up to 2.5 g/kg/day to meet the nitrogen balance created by the hypercatabolic state of acute renal failure and protein losses during filtration.
Complications
Complications of TPN can be organized into three groups: administration/venous access, metabolic complications, and others.7,8,10
Administration/Venous Access
- TPN should be given through a dedicated port on a central line due to its incompatibility with multiple medications, increased risk for infection, and high osmolarity leading to irritation of peripheral veins. Risks associated with central line placement and indwelling catheters:
- Pneumothorax
- Air embolism
- Bleeding
- Vascular injury
- Venous thrombosis
- Infections (more common with TPN than other infusions due to content and immunocompromised status of patients needing PN)
- Central line-associated bloodstream infections
- Local skin infection at the insertion site
Metabolic Complications
- Refeeding syndrome occurs in patients with chronic alcoholism or previously nil per os for greater than 7-10 days. This presents as hypophosphatemia, hypomagnesemia, hypokalemia, and hyperinsulinemia.
- Hyperglycemia
- Hypoglycemia (occurs with sudden discontinuation)
- Serum electrolyte abnormalities
- Acid-base disturbances
- Hypertriglyceridemia
- Carnitine deficiency
Other Complications
- Hypervolemia
- Wernicke’s encephalopathy
- Pancreatitis
- Parenteral-associated cholestasis (reversible, due to overfeeding)
- Hepatic steatosis (fatty infiltration of the liver from overfeeding)
- Compromise of gut integrity, bacterial translocation
- Essential fatty acid deficiency
- Presents with dermatitis, alopecia, poor wound healing, increased platelet aggregation, increased capillary fragility, hepatic dysfunction
Anesthetic Considerations
- Patients receiving TPN are often critically ill and require surgical procedures. During the perioperative period, it is important to monitor the patient closely for the complications noted in the previous section, in addition to the following perioperative considerations.
- The infusion of TPN should be continued whenever possible due to the risk of hypoglycemia with sudden discontinuation.
- Metabolic abnormalities are common and ideally should be corrected preoperatively.
- To minimize the risk of infection, the infusion should remain connected to a dedicated port of a central venous catheter.
- Frequent glucose monitoring is important in all procedures to identify and treat both hypoglycemia and hyperglycemia. Hypoglycemia is common with the abrupt discontinuation of TPN. Hyperglycemia can occur with continued TPN administration in addition to the neuroendocrine stress response from surgery.10
- Hypophosphatemia can contribute to muscle weakness and postoperative respiratory failure due to adenosine triphosphate depletion.
- TPN is a significant source of volume intake. Care must be taken to adjust intravenous fluid infusion rates to achieve euvolemia.7
References
- Berlana D. Parenteral nutrition overview. Nutrients. 2022;14(21):4480. PubMed
- Martínez-Ortega AJ, Piñar-Gutiérrez A, Serrano-Aguayo P, et al. Perioperative nutritional support: A review of current literature. Nutrients. 2022;14(8):1601. PubMed
- American Gastroenterological Association. American Gastroenterological Association medical position statement: short bowel syndrome and intestinal transplantation. Gastroenterology. 2003;124(4):1105-10. PubMed
- McClave SA, DiBaise JK, Mullin GE, Martindale RG. ACG clinical guideline: Nutrition therapy in the adult hospitalized patient. Am J Gastroenterol. 2016;111(3):315-335. PubMed
- Cederholm T, Bosaeus I. Malnutrition in adults. N Engl J Med. 2024;391(2):155-65. PubMed
- Lewis SR, Schofield-Robinson OJ, Alderson P, Smith AF. Enteral versus parenteral nutrition and enteral versus a combination of enteral and parenteral nutrition for adults in the intensive care unit. Cochrane Database Syst Rev. 2018;6(6):CD012276. PubMed
- Chowdary KRV, Reddy PN. Parenteral nutrition: revisited. Indian J Anaesth. 2010; 54(2): 95-103. PubMed
- Slattery E, Rumore MM, Douglas JS, Seres DS. 3-in-1 vs 2-in-1 parenteral nutrition in adults: a review. Nutr Clin Pract. 2014;29(5):631-5. PubMed
- Braga M, Ljungqvist O, Soeters P, et al. ESPEN guidelines on parenteral nutrition: surgery. Clin Nutr. 2009;28(4): 378-386. PubMed
- Nutrition in Perioperative & Critical Care. In: Butterworth IV JF, Mackey DC, Wasnick JD. eds. Morgan & Mikhail's Clinical Anesthesiology, 6e. McGraw-Hill Education; 2018. Accessed June 18, 2025. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.