Copy link
Perioperative Infection Risks
Last updated: 05/15/2024
Key Points
- Surgical site infections (SSIs) comprise approximately 20% of all healthcare-associated infections (HAIs) and inflict substantial financial burdens, as well as mortality risks.
- Both modifiable and nonmodifiable factors related to patients and surgical procedures influence the risk of SSIs.
- Implementing antimicrobial prophylaxis is essential to thwart SSIs, while evidence-based infection control protocols in the anesthesia domain can markedly diminish the transmission of pathogens, thereby enhancing patient safety.
Perioperative Infection Types
- HAIs are categorized broadly by the Centers for Disease Control and Prevention into:
- Central line-associated bloodstream infections (CLABSI)
- Catheter-associated urinary tract infections (CAUTI)
- Surgical site infections (SSI)
- Ventilator-associated pneumonia (VAP)
- In surgical settings, SSIs are the primary concern, yet perioperative teams also confront the risk of other nosocomial infections among patients transitioning to postoperative care.
- Incidence and impact of SSIs1-3:
- SSIs develop in incisional wounds and typically present at a rate of 2-5% within 30 days of surgery or 90 days of implanted devices.
- Despite constituting approximately 20% of all HAIs, SSIs are financially burdensome:
- SSIs prolong hospital stays by an average of 9.7 days.
- SSIs escalate admission costs by over $20,000 per patient.
- SSIs correlated with a 2- to 11-fold rise in mortality risk, with 75% of SSI-related deaths directly attributable to the infections.
- Classification and clinical presentation of SSIs2:
- SSIs are classified by depth into superficial-incisional, deep-incisional, and organ/space infections.
- Clinical presentations vary but commonly include incisional site abnormalities, such as redness, delayed healing, fever, pain, tenderness, warmth, swelling, or drainage.
- Prevalent pathogens causing HAIs:1
- Enterococcus, Staphylococcus aureus (including methicillin-resistant strains like MRSA), Klebsiella, Acinetobacter, Pseudomonas, and Enterobacter spp. (collectively called ESKAPE organisms)
- MRSA is considered a primary culprit for SSIs in the United States.
Surgical Site Infection Risk Assessment
Wound Classification2,4
- The type of surgical procedure represents a notable risk factor for postoperative complications, particularly wound infections. Surgical procedures are categorized into four groups based on the degree of wound contamination: clean, clean-contaminated, contaminated, and dirty-infected. Each category carries varying rates of postoperative wound infections, with an escalating trend in SSI rates from clean to dirty-infected wounds (Table 1).
- Antibiotic prophylaxis is recommended for most clean-contaminated procedures, while therapeutic antibiotic use is indicated for contaminated procedures or cases of established infections.
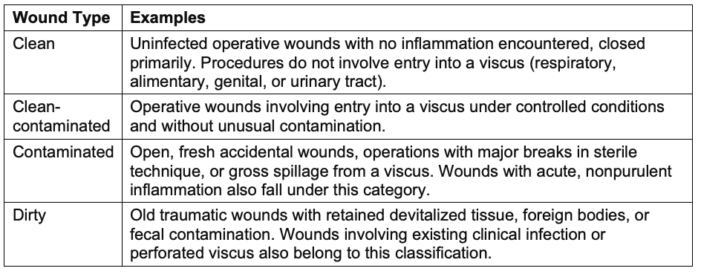
Table 1. Wound classification and definition
Risk Factors
- The occurrence of SSIs is contingent upon a multifaceted interplay of several factors, such as the type and quantity of organisms present at the surgical site, the overall health status of the patient, and the proficiency of the surgical technique.
- These risk factors can be categorized as modifiable and nonmodifiable patient-related and operation-related factors, each associated with distinct pathophysiologies.4 Tables 2 and 3 describe these risk factors.
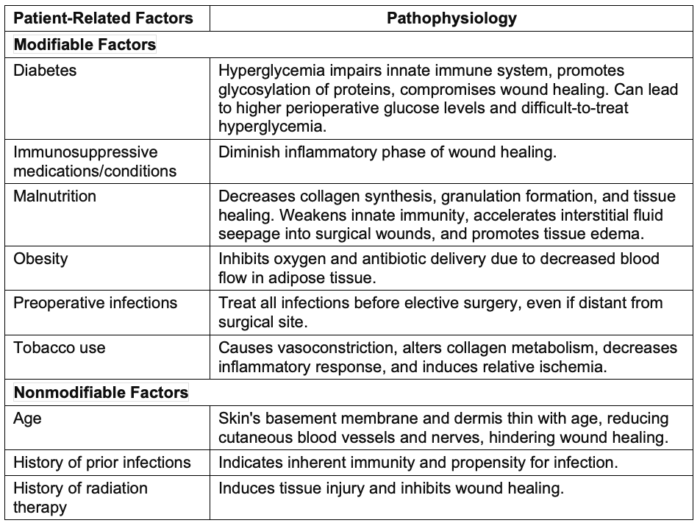
Table 2. Modifiable and non-modifiable patient-related factors for SSIs. Adapted with permission from Seidelman JL, et al. Surgical site infection prevention: A review. JAMA. 2023.
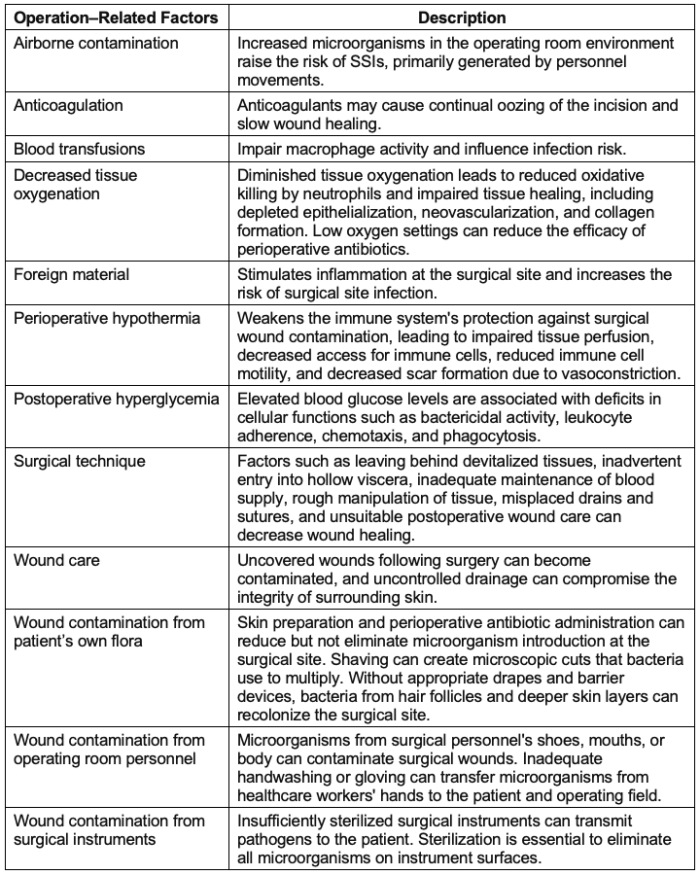
Table 3. Modifiable operation-related factors for SSIs. Adapted with permission from Seidelman JL, et al. Surgical Site Infection Prevention: A Review. JAMA. 2023
SSI Prophylaxis
Causative Pathogens of SSI
- SSIs can arise from various bacterial sources, depending on the nature of the surgical procedure.2,4
- Adherence to institutional pharmacy and surgical antimicrobial prophylaxis guidelines is crucial.
- SSIs are commonly attributed to skin flora, including streptococcal species, staphylococcus aureus, and coagulase-negative staphylococci.
- Gram-negative rods and enterococci prevail alongside skin flora in clean-contaminated procedures.
- Pathogens mirror the endogenous flora of involved viscera or adjacent mucosal surfaces.
Antibiotic Choices2,4
- Cefazolin is commonly chosen for its efficacy, safety, and cost-effectiveness. It exhibits activity against streptococci, methicillin-susceptible staphylococci, and numerous gram-negative organisms.
- Vancomycin or clindamycin may serve as alternatives in certain circumstances, especially for a higher risk of MRSA infection.
Antibiotic Administration2,4
- Antibiotics are recommended within 60 minutes before surgery to achieve adequate serum and tissue concentrations.
- Intraoperative dosing repetition until wound closure is advised for procedures exceeding two half-lives of the drug or involving substantial blood loss.
- Limiting prolonged postoperative antibiotic usage is essential to mitigate the risk of antibiotic resistance and acute kidney injury.
- Infection control measures span across perioperative care5 (Figure 1) and can significantly reduce pathogen transmission and lower SSI risk.
- Recommended interventions target key infection routes3,5 (Table 4):
- Direct wound contamination
- Spread from patient skin colonization
o Aerosolization from anesthesia work area reservoirs
o Hematogenous spread from contaminated injection ports, syringe tips, or medication vials.
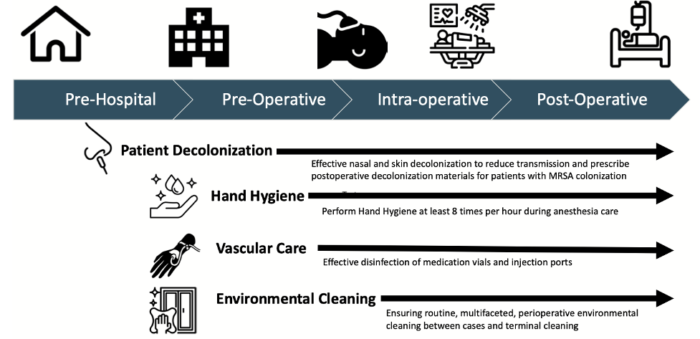
Figure 1. Evidence-based high-value opportunities to mitigate transmission of infection across the perioperative continuum. Reproduced with permission from Charnin JE, Hollidge M, Bartz R, et al. A A Best Practice for Anesthesia Work Area Infection Control Measures: What Are You Waiting For? APSF Newsletter 2022;37:103-106.
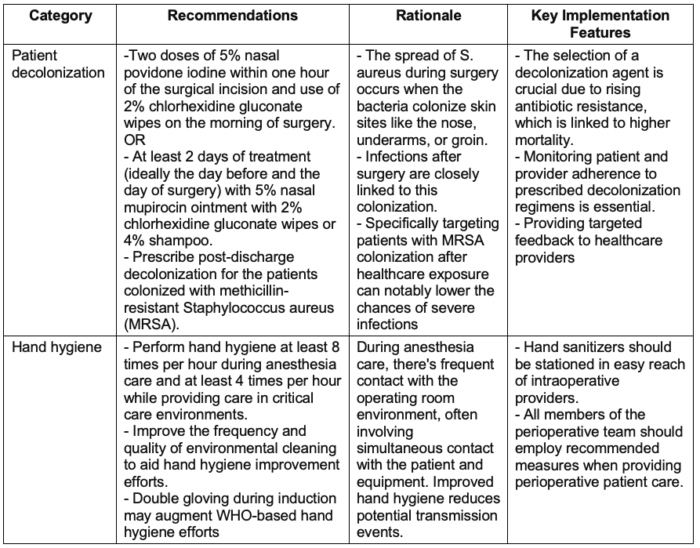
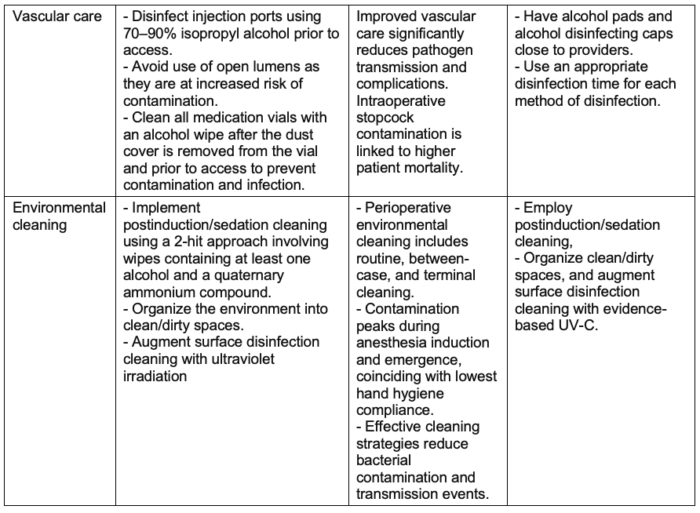
Table 4. Multimodal perioperative infection control. Used with permission from Charnin JE et al. A best practice for anesthesia work area infection control measures: what are you waiting for? APSF Newsletter. 2022.
References
- Monegro AF, Muppidi V, Regunath H. Hospital-acquired infections. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; Accessed April 28, 2024. Link
- Anderson DJ. Antimicrobial prophylaxis for prevention of surgical site infection in adults. In Post T (ed): UpToDate; 2024. Accessed April 28, 2024. Link
- Simmons CG, Hennigan AW, Loyd JM, et al. Patient safety in anesthesia: Hand hygiene and perioperative infection control. Curr Anesthesiol Rep. 2022;12(4):493-500. PubMed
- Seidelman JL, Mantyh CR, Anderson DJ. Surgical site infection prevention: A review. JAMA. 2023;329(3):244-52. PubMed
- Charnin JE, Hollidge M, Bartz R, et al. A best practice for anesthesia work area infection control measures: what are you waiting for? APSF Newsletter. 2022; 37:103-6. Link
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.