Copy link
Perioperative Infection Prevention
Last updated: 04/02/2025
Key Points
- Central venous catheter (CVL) infection causes significant morbidity and mortality.
- Center for Disease Control (CDC) and Prevention guidelines for CVL infection prevention include seven key components and recommendations: education, CVL site selection, hand hygiene, skin preparation, barrier precautions, dressing, and timing of CVL replacement.1
- Contamination of the anesthesia work area, including anesthesia carts, computers, ventilators, and other supplies, can result in transmission to the patient, resulting in healthcare-associated infections and increased risk of patient mortality. Fortunately, steps can be taken to reduce these risks.2,3
Central Line Infection Facts
- Infection is a serious late complication of CVL placement
- An estimated 250,000 cases of catheter-related bloodstream infections occur per year.4
- The mortality of nosocomial bloodstream infections is 35%.
- The cost of one catheter-related bloodstream infection is roughly $46,000.4
- In the United States, the CLABSI rate in intensive care units (ICU) is estimated to be 0.8 per 1000 central line days.4
CDC Guidelines for Infection Prevention for Central Venous Lines1
- The CDC’s most recent prevention guidelines encompass seven key components imperative to infection prevention.1 The guidelines are categorized into:
- 1A recommendations (highly recommended and has supporting evidence);
- 1B (strongly recommended and some evidence); and
- 1C is required by regulatory agencies, and category II is suggested for future implementation.
- Table 1 below shows CDC recommendations for CVLs, along with their corresponding level of evidence.
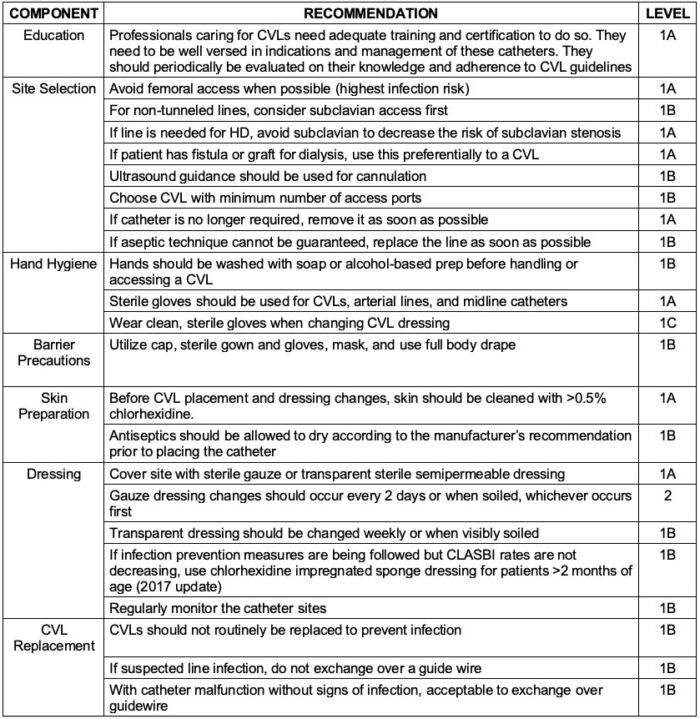
Table 1. CDC recommendations for central line infection prevention. Adapted from O’Grady et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. October 2017.
- According to the ASA’s recently published revision of Recommendations for Infection Control for the Practice of Anesthesiology, the following are additional steps to reduce infection transmission with catheters in situ.3
- Disinfectable, needleless closed connection ports (DNCCPs) should be used to prevent entrainment of environmental air while allowing for continued intravenous (IV) use.
- Open stopcocks need to be closed or connected to a DNCCP.
- Prior to accessing ports in an IV circuit, they should be scrubbed with a 70% isopropyl alcohol wipe for 5-15 seconds and allowed to air dry for 5 seconds prior to use.
Anesthesia Workstation Infection Prevention
- Anesthesia providers perform certain actions across a variety of settings that are concerning for infection (Figure 1).2
- These “problematic practices” can include:
- the use of multiple-dose vials for more than one patient;
- lack of glove use during airway management; and
- failure to perform proper hand hygiene (including after removing gloves, before and after airway and line management, and prior to entry into anesthesia carts).

Figure 1. Infection prevention by anesthesia providers. Reproduced and modified with permission from Charnin et al. A Best Practice for Anesthesia Work Area Infection Control Measures: What Are You Waiting For? APSF Newsletter. 2022; 37 (3);1-4.
- What are appropriate moments in anesthesia management to perform proper hand hygiene?2,3
- At a minimum:
1. Before aseptic tasks (IVs, art lines, drawing up medications)
2. After removing gloves or prior to donning sterile gloves
3. When hands are soiled or contaminated
4. Before touching the contents of the anesthesia cart
5. When entering or exiting the operating room
6. After touching bodily fluids
- At a minimum:
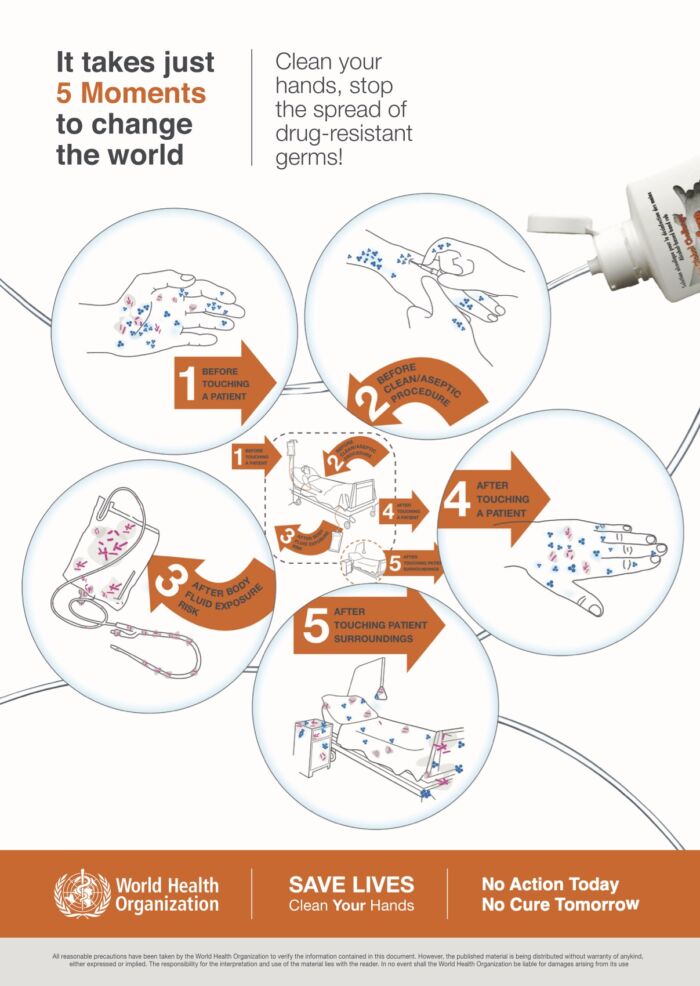
- The World Health Organization (WHO) recommends five moments for hand hygiene to prevent infections (Figure 2).
- Hand hygiene steps are depicted in Figure 3.
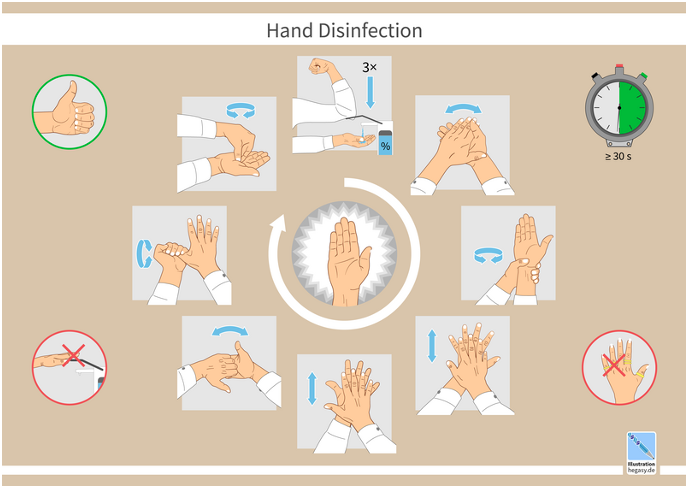
Figure 3. Hand hygiene steps. Adapted from: Guido4, Wikimedia Commons. Link CC BY-SA 4.0
- Table 2 summarizes other recommendations for proper infection prevention in the anesthesia work area.2,3
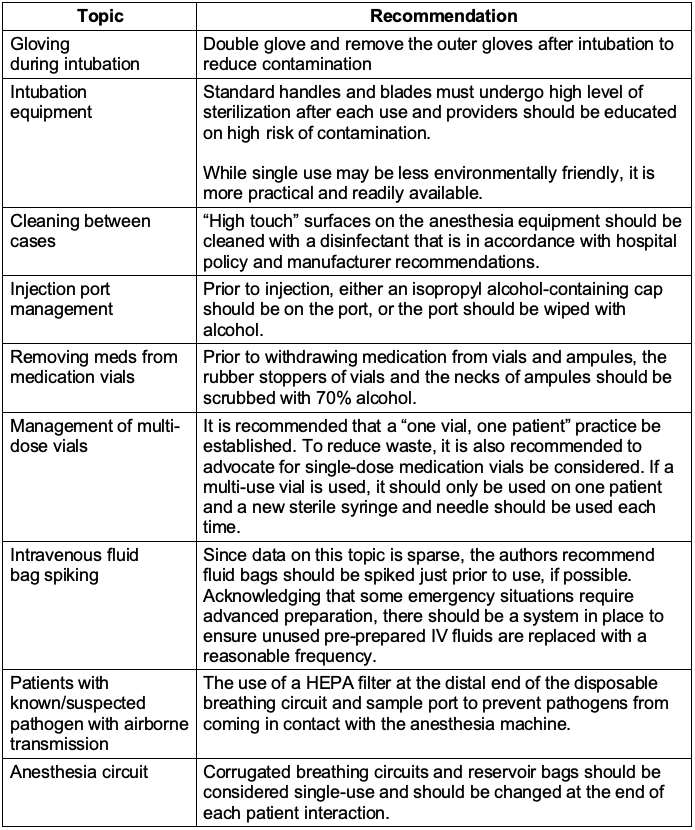
Table 2. Recommendations for infection prevention in the anesthesia work area.
References
- O’Grady, NP, Alexander M, Burns LA, et al. Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. October 2017. Accessed March 11, 2025. Link
- Munoz-Price LS, Bowdle A, Johnston BL, et al. Infection prevention in the operating room anesthesia work area. Infect Control Hosp Epidemiol. 2019;40(1):1-17. PubMed
- Beers R, et al. Recommendations for infection control for the practice of anesthesiology: Preventing infectious transmission during anesthesia care. American Society of Anesthesiologists. Asahq.org. Revised February, 2024. Accessed March 18, 2025. Link
- Haddadin Y, Annamaraju P, Regunath H. Central line–associated blood stream infections. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024. Accessed March 11, 2025. Link
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.