Copy link
Perioperative Handovers
Last updated: 11/20/2024
Key Points
- Transitions of care are often associated with patient harm and are an area of focus for healthcare regulatory agencies.1
- Many institutions have implemented standardized handoff checklists for intraoperative and postoperative locations, reducing the amount of information omitted during sign-outs.
- Establishing a standardized, institutional handoff guideline will increase consistency in the information provided during transitions of care.
Introduction
- The Anesthesia Patient Safety Foundation (APSF) convened a group of experts to develop a consensus statement regarding six areas of perioperative handoffs and their safety implications:2
- Process elements and behaviors
- Metrics and measurement
- Important research questions
- Best ways to manage training and education
- How best to implement
- How to incorporate patient and family goals into handoffs.
- Standardization and use of checklists during handoffs have improved communication, patient care, and safety during intraoperative handoffs.3
- Some institutions use standardized handoff checklists to ensure consistent information is shared during handoff. One method is SBAR (situation, background, assessment, recommendation).1
Process Elements and Behaviors
- There are many necessary process elements and behaviors to be adopted.
- Incorporating these behaviors during handoff periods improves the quality of the handoff. It allows precise and undistracted transfer of information, which leads to enhanced care in the next phase of the clinical course.
- The APSF consensus statement recommends the following behaviors during handoffs:2
- Interruptions and distractions should be minimized during the handoff.
- Adequate time should be allotted, with an explicit expectation for participants to ask questions and raise concerns.
- Information transfer should be thorough yet concise.
- Communication during handoffs should be clear, concise, consistent, and interactive.
- All participants should be receptive to questions and concerns.
- All participants should act with mutual respect and practice positive teamwork, establishing role clarity, willingness to collaborate, and equality of value of others’ information.
- The handoff should have a structured or standardized process.
- One person should speak at a time.
- All participants should have had handoff education and training.
Metrics and Measurements
- Measuring and quantifying the effectiveness and impact of perioperative handoff is important to continue improving the process.
- The APSF consensus statement recommends the following metrics for the assessment of the perioperative handoff process:2
- Morbidity (including major adverse effects) and mortality
- Efficiency and time-related process
- Measures related to handoff process implementation
- Hospital quality indicators and preventable adverse safety events
- Information transfer (e.g., information omissions or inclusions, completeness/thoroughness of communication)
Handoff Research
- The following questions help those interested in handoff research to focus their effort and provide guidance to organizations that provide funding for these endeavors.2
- What factors impact handoff failure and success?
- What is the impact of handoffs on process and patient outcomes?
- How should handoff quality be assessed?
- What is the role of cognitive support tools (both physical and electronic) in handoff success or failure
- What are the best practices for conducting safe and effective handoffs?
- What are the current attitudes and beliefs of healthcare professionals toward the importance of a structured handoff process?
Managing Training and Education
- Although education and training on handoffs alone are insufficient, they are essential in creating an environment for safe perioperative care.
- The APSF consensus statement recommends the following regarding training and education:2
- The development of the handoff education and training program should include all stakeholders and be supported by leadership.
- Handoff education and training should include feedback about handoff performance.
- Leaders should ensure the development of education and training for effective handoffs.
- Handoff education and training should impart the value of an effective handoff and should help learners understand the consequences of a poor handoff.
- Handoff education and training should include ongoing observation, real-time coaching, and feedback.
- Handoff education and training should occur early in one’s training and on an evolving basis throughout one’s career.
Implementation
- Successful implementation of new handoff processes requires early engagement of key stakeholders.
- The process should be multidisciplinary and involve champions in each relevant discipline.
- The APSF consensus statement recommends the following regarding how to best implement new handoff processes:2
- Interprofessional teams should collectively design a reliable method for information transfer in a manner that promotes teamwork.
- Clinical units and departments should apply quality improvement principles to handoff redesign.
- Trained observers should periodically evaluate handoffs to provide feedback to participants.
- All stakeholders should be engaged early in the process to elicit buy-in, as well as concerns and barriers.
- Site leads and unit-based champions should be identified, trained, and mentored to ensure their respective peers understand the intent and purpose of the redesign effort.
Patient and Family Engagement
- Patients and family members are usually not involved in handoffs due to obvious challenges in the busy perioperative setting.
- However, given the importance of patient-centered care and the potential influence of handoffs on patient care satisfaction, patients and families should be encouraged to participate, depending on the setting and acuity of the patient.
- Patients and families should also have a mechanism to communicate issues via a hotline or quality improvement reporting mechanism if they cannot be present.
Using the Electronic Medical Record (EMR)
- Intraoperative handoffs can occur during breaks or when there is a complete transfer of care (e.g., at the end of a shift or when the clinician is deployed for another assignment).
- Some institutions use an intraoperative handoff checklist embedded in EMR to streamline the process.
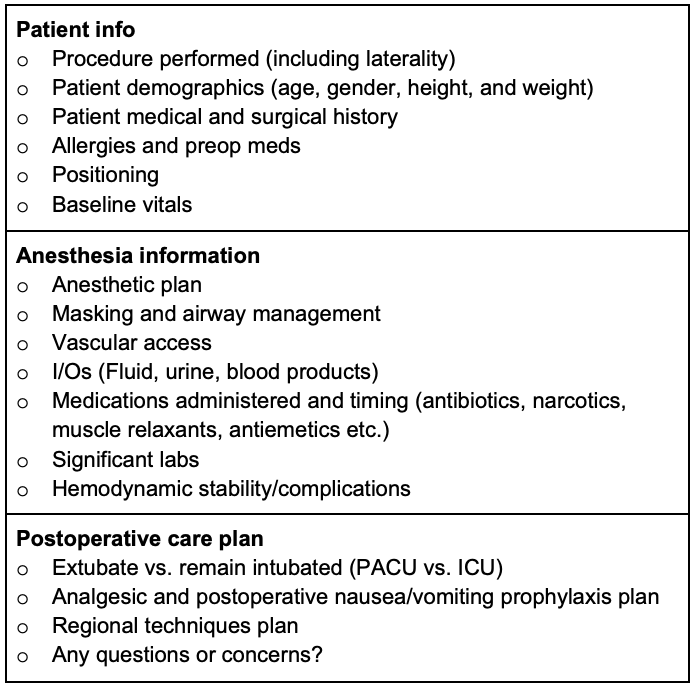
Table 1. An example of an intraoperative handoff checklist
Examples of Handoff Checklists
- Handoff protocol/checklist for the postanesthesia care unit (PACU)1
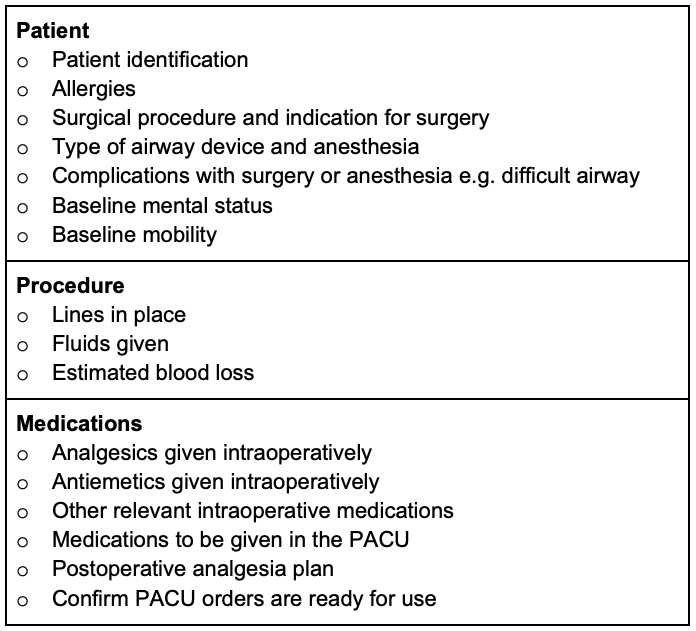
Table 2. Checklist for PACU handoff. Adapted from Potestio C. Improving Post Anesthesia Care Unit (PACU) Handoff by Implementing a Succinct Checklist. Anesthesia Patient Safety Foundation, June 2015.
- Handoff of surgical patients in the intensive care unit (ICU)
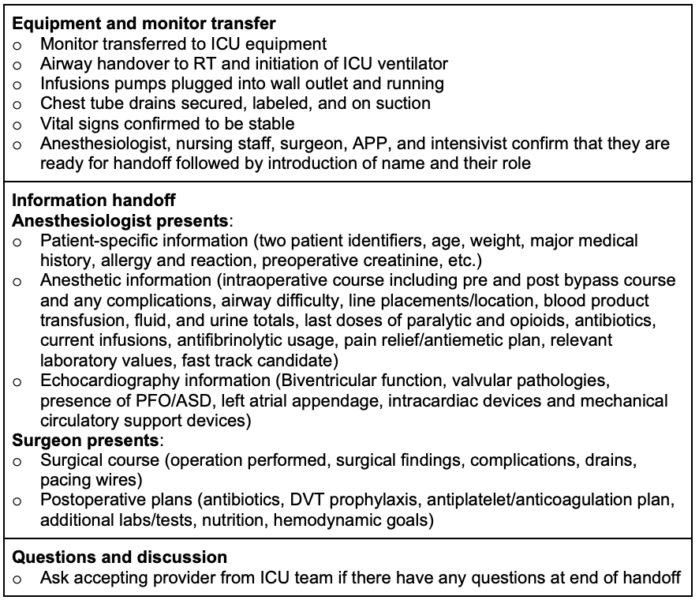
Table 3. Example of a cardiovascular ICU handoff checklist
References
- Potestio C, Mottla J, Kelley E, et al. Improving post-anesthesia care unit (PACU) handoff by implementing a succinct checklist. Anesthesia Patient Safety Foundation Newsletter, June 2015, Accessed Nov 03, 2024. Link
- Agarwala AV, Lane-Fall MB, Greilich PE, et al. Consensus recommendations for the conduct, training, implementation, and research of perioperative handoffs. Anesth Analg. 2019;128(5):e71-e7. PubMed
- Petrovic MA, Martinez EA, Aboumatar H. Implementing a perioperative handoff tool to improve postprocedural patient transfers. J Comm J Qual Patient Saf 2012; 38:135–142. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.