Copy link
Pediatric Obesity
Last updated: 07/01/2024
Key Points
- The global epidemic of obesity is a serious public health crisis affecting both adults and children.
- Pediatric obesity is associated with several comorbidities including hypertension, diabetes, metabolic syndrome, obstructive sleep apnea, etc.
- Obese patients should be positioned in the ramped position for laryngoscopy, or the head of the bed should be elevated by 25-30 degrees.
- Obese children are at an increased risk of perioperative respiratory adverse events and must be monitored closely.
Prevalence
- Pediatric obesity is a global public health emergency that poses a massive burden on the healthcare system.1
- In 2016, it was estimated that there were 42 million obese children younger than 5 years of age worldwide.2 In the United States, one in five children was obese or overweight in 2016.1 The prevalence of pediatric obesity is increasing significantly, especially in developing countries.
- As pediatric obesity becomes more prevalent, anesthesia providers must become more familiar with the perioperative considerations and comorbid conditions associated with pediatric obesity.
Definitions
- The body mass index (BMI) is a common screening tool for obesity. It is calculated by dividing the patient’s weight in kilograms by the square of the height in meters. BMI can be erroneously high in patients with increased muscle mass or shorter stature and, conversely, can be lower in patients with lower muscle mass from inactivity.1 Despite its flaws, BMI is commonly used to classify obesity in adults.
- In children, BMI varies with age, sex, and maturity, making its interpretation difficult. Therefore, a child’s BMI is entered on gender-specific growth charts to calculate the BMI-for-age percentiles. Cutoffs of 85th, 95th, and 99th percentile are used to classify overweight, obesity, and severe obesity in children. Clinically, any child with a BMI ≥ 35 kg/m2 or a BMI ≥ 120% of the 95th percentile is classified as severely obese1 (Table 1).
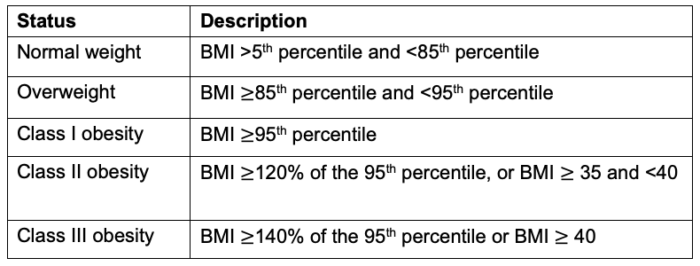
Table 1. Classification of pediatric obesity
Medical Comorbidities
Cardiovascular
- Hypertension: Obese children and adolescents are at a significantly increased risk (2.5-3.7 times more likely) of having elevated blood pressure.4 Poorly controlled or undiagnosed hypertension can result in highly labile intraoperative blood pressure.2
- Left ventricular hypertrophy: Uncontrolled hypertension can lead to ventricular hypertrophy which results in increased myocardial oxygen demand.4
- Atherosclerosis and coronary artery disease: Although atherosclerosis is believed to only occur in adults, recent studies of pediatric vasculature show fatty deposition and carotid intima-media thickening in obese adolescents and children.4
- Pulmonary hypertension and right ventricular dysfunction: Patients with undiagnosed and untreated obstructive sleep apnea (OSA) can develop pulmonary hypertension from nocturnal hypoxemia.1-3 This can lead to issues with oxygenation and right ventricular function perioperatively.
- Cardiology should be consulted for obese patients with uncontrolled systemic hypertension, signs of right ventricular dysfunction, and multiple episodes of nocturnal desaturations below 70%.2
Respiratory
- Perioperative respiratory adverse events are the leading cause of morbidity and mortality in pediatric anesthesia.
- Asthma: Reactive airway disease and asthma are present in roughly one-third of obese children and can lead to perioperative respiratory adverse events, such as bronchospasm and laryngospasm.
- OSA: Depending on which study is cited, OSA is present in between 13-59% of obese children compared to only 1-2% of normal-weight children.2 The increased risk of OSA in obese children is secondary to multiple causes, including adenotonsillar hypertrophy, airway narrowing, increased critical airway closing pressures, abnormal ventilatory control, and decreased chest wall compliance.2
- For every 1 kg/m2 increase in BMI, the risk of OSA increases by 12%.2 Undiagnosed OSA can lead to decreased CO2 sensitivity and compensated chronic respiratory acidosis. Additionally, as discussed earlier, OSA is a risk factor for developing pulmonary hypertension and right ventricular dysfunction in severe cases.
- Therefore, obese children should be routinely screened for OSA (see OA Summary on pediatric OSA). Link While polysomnography is the gold standard for diagnosing OSA, most children with OSA have not undergone a preoperative polysomnography.
Gastrointestinal
- Gastroesophageal reflux disease (GERD): Although GERD is more common (roughly 10 times more common in obese children than normal-weight children), fasting duration, and gastric residual volumes are not statistically significant. Therefore, fasting guidelines for obese children are the same as nonobese children and appropriately fasted obese children do not require a rapid sequence induction. Although GERD is associated with obesity, it does not appear to be an independent risk factor for increased aspiration risk in obese children.1
- Nonalcoholic fatty liver disease: Nonalcoholic fatty liver disease (NAFLD) is the most prevalent form of pediatric liver disease and is usually asymptomatic. Studies report nearly 50% of obese children have some fatty deposition in their liver, while up to 3% may have progressed to the most severe form of nonalcoholic steatohepatitis (NASH).4 Although weight loss is the mainstay of treatment in adults, current treatment in children is still being studied. NAFLD and NASH can impact synthetic liver function when in their most severe form, altering drug metabolism.
Endocrine
- Insulin resistance: Patients with increased adiposity are at a higher risk for developing insulin resistance, leading to hyperinsulinemia that can cause hypertension and hypercholesterolemia.4
- Dyslipidemia: It is prevalent in 5-10% of pediatric patients and is higher in obese patients. It can worsen other conditions, including insulin resistance, type II diabetes, atherosclerosis, and metabolic syndrome.
- Type II diabetes: Originally thought to be adult onset, recent studies show that nearly half of all new diagnoses of diabetes in pediatric patients are from type II diabetes.4 Patients with diabetes require additional blood glucose monitoring intraoperatively.
- Metabolic syndrome: Metabolic syndrome is diagnosed in the presence of three of the following five criteria — elevated triglycerides, low high-density lipoprotein, central obesity/abdominal circumference by sex, elevated fasting glucose, and high blood pressure. Metabolic syndrome is a risk for cardiovascular disease and diabetes.4 The odds of developing metabolic syndrome are increased 1.5 times for every half-unit increase in BMI.2
- Polycystic ovarian syndrome (PCOS): Obese adolescent girls are at an increased risk for hyperandrogenism and early onset PCOS, which is characterized by menstrual irregularities, hirsutism, acne, and obesity. PCOS is strongly associated with insulin resistance and is a major risk factor for the development of metabolic syndrome and type II diabetes in women.
Skeletal
- Orthopedic issues such as slipped capital femoral epiphysis (nontraumatic displacement of the proximal femoral epiphysis from the metaphysis) and tibia vara or Blount’s disease (bowed legs, abnormal gait) are more common in obese children and adolescents.
Psychosocial
- Psychosocial consequences of pediatric obesity are widespread. The risk of psychosocial issues increases with age and girls are at greater risk than boys. Symptoms of depression and lower self-esteem are higher among obese adolescents. Overweight and obese adolescents are frequent targets of teasing and bullying, and they are more likely to be socially marginalized.
- Obese children and adolescents report significantly lower health-related quality of life (QOL) scores than normal-weight peers and similar QOL scores as those diagnosed with cancer.
Anesthetic Challenges
Airway Management
- Difficult mask ventilation: Obesity is a risk factor for difficult mask ventilation due to increased soft tissue in the neck that causes significant obstruction during mask ventilation, especially when patients are paralyzed.1-3
- Difficult laryngoscopy: Obese children are more likely to have larger neck circumferences, which increases the risks of difficult laryngoscopy.
- To optimize intubating conditions, obese patients should be positioned in the “ramped” position (with the patient’s external auditory meatus at the same level as the sternum) or the head of the bed elevated 25-30 degrees. If appropriate ramped positioning is utilized, there is no statistically significant difference in the success of direct laryngoscopy in obese children and adolescents.3
- Restrictive pulmonary pattern: Obese children have decreased functional residual capacity and forced vital capacity and are prone to hypoxemia in the supine position.1-3 Fat accumulation in the chest wall decreases lung and chest wall compliance and increases the work of breathing.2
- Preoxygenation: Prior to induction of anesthesia, adequate preoxygenation is recommended in obese patients. Tidal breathing for 3 minutes with 100% oxygen is recommended in obese children. In obese adults, preoxygenation for 5 minutes with 100% oxygen with a continuous positive airway pressure of 10 cm H2O, mask ventilation with a positive end-expiratory pressure (PEEP) of 10 cm H2O, and the 25 degrees head-up position has been shown to increase the time to saturation.2
- Intraoperative ventilation: A lung-protective ventilation strategy is recommended that includes tidal volumes of 6-8 mL/kg ideal body weight, modest levels of PEEP (5-15 cm H2O and titrated up as needed), fraction of inspired oxygen below 0.5 and 0.8, and intermittent use of alveolar recruitment maneuvers, if needed.2
- Extubation: During emergence, the obese patient must be positioned in the head-up position and extubated when fully awake.
Monitoring and Vascular Access
- Obese children pose several monitoring challenges.1-3 Appropriately sized blood pressure cuffs should be used and using alternative cuff sites, such as the forearm and calf, may be necessary. Arterial lines and central venous catheters are rarely needed in the absence of severe cardiovascular disease.3
- Excessive subcutaneous adipose tissue accumulation results in low-voltage EKG signals and complicates neuromuscular blockade monitoring as well. End-tidal CO2 levels may not always correlate with PaCO2 levels in obese patients secondary to decreased functional residual capacity and ventilation-perfusion mismatch.
- Obtaining vascular access can be challenging in obese children and ultrasonography can be invaluable in this setting.3 Few studies exist describing challenges with obtaining vascular access in obese pediatric patients. A study in critically ill patients showed that obese children were more likely to receive central venous access.1
Patient Positioning
- Obese patients may require extra assistance in transferring to the operating room table. Caring for obese patients may lead to injury among operating room staff when lifting them to and from the operating room table.1
- Additionally, these patients will require “ramped” positioning or the head of the bed elevated to optimize intubation conditions.1 Supine position and Trendelenburg’s positions must be avoided in obese patients secondary to the exaggerated reduction in lung volumes from cephalad displacement of the diaphragm. In addition, these positions can result in increased venous return, cardiac output, pulmonary blood flow, and arterial blood pressure.
- The obese patient’s extremities must be well-padded to prevent peripheral nerve injuries.2
Perioperative Analgesia
- To minimize the risk of opioid-induced respiratory depression, a multimodal approach is recommended, including regional anesthesia or local anesthetic wound infiltration, acetaminophen, ketorolac, dexmedetomidine, etc.2
Postoperative Complications
- Obese children are at an increased risk for postoperative complications, including upper airway obstruction, laryngospasm, bronchospasm, and desaturation.1-3 Unplanned hospital admissions and postanesthesia care unit length of stays are higher in obese children.
- Patients with OSA should be closely monitored postoperatively. Noninvasive ventilation (continuous positive airway pressure or bilevel positive airway pressure) may be necessary.
- Surgical site infections are more common in obese patients. Therefore, adequate antibiotic coverage should be ensured.
- Venous thromboembolic events (VTE), such as deep venous thrombosis and pulmonary embolism, are more common in obese patients.1 Unfortunately, there is a paucity of data regarding VTE prophylaxis in obese children.
Anesthetic Drug Dosing
- Obesity affects the pharmacokinetics of several anesthetic drugs. Please see the OA Summary on drug dosing in patients with obesity for more details. Link
- Briefly, several dosing scalars are used to calculate drug dosage, including total body weight (TBW), lean body weight (LBW), and ideal body weight (IBW). LBW (or fat-free mass) is the difference between TBW and fat mass and consists of vital organs, muscle, bone, and extracellular fluid. Obesity is associated with an increase in both fat mass and absolute lean mass, with the increase in lean mass accounting for 20% to 40% of the excess weight. However, fat mass and lean mass do not increase proportionally, and with increasing obesity, the LBW/TBW ratio decreases.
- LBW has been suggested as the ideal scalar for calculating drug dosage in obese patients. Cardiac output, a key determinant of a drug’s early distribution kinetics, strongly correlates with LBW.
- IBW in children is commonly calculated using the BMI method, which involves multiplying the BMI at the 50th percentile for that child’s age by the square of height (in meters).
- Several online calculators are available to calculate a patient’s LBW. Some examples include www.calculator.net Link and www.paedspro.com Link.
- Normograms for calculating IBW and LBW have been developed. Please see reference 5.
References
- Mpody C, Owusu-Bediako K, Raman VT, et al. Pediatric obesity and perioperative medicine. Curr Opin Anaesthesiol. 2021; 34(3):299-305. PubMed PubMed
- Chidambaran V, Tewari A, Mahmoud M. Anesthetic and pharmacologic considerations in perioperative care of obese children. J Clin Anesth. 2018; 45:39-50. PubMed
- Samuels PJ, Sjoblom MD. Anesthetic considerations for pediatric obesity and adolescent bariatric surgery. Curr Opin Anaesthesiol. 2016; 29(3): 327-36. PubMed
- Daniels SR. The consequences of childhood overweight and obesity. Future Child. 2006; 16(1): 47-67. PubMed
- Callaghan LC, Walker JD. An aid to drug dosing safety in obese children; development of a normogram to determine ideal and lean body mass. Anaesthesia. 2015; 70:176-82. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.