Copy link
Pediatric Airway Evaluation
Last updated: 04/26/2023
Key Points
- A comprehensive airway evaluation is a critical component of airway management in both children and adults.
- Pediatric patients are especially vulnerable to adverse respiratory events during anesthesia. A thorough history and a focused physical examination of the pediatric airway is an invaluable tool to assess the possibility of a difficult airway and ensure necessary equipment is readily available.
History1,2
A comprehensive airway history should include the following:
- past medical history and birth history (e.g., history of prematurity, craniofacial syndrome, neuromuscular disease, etc.)
- airway-related comorbidities (e.g., respiratory illness, aspiration, phonation, airway injuries)
- prior airway management/complications during anesthesia
- surgical procedures involving the airway.
Birth History
- This should include details of the child’s birth, hospitalization, prior airway management/support, need for supplemental oxygen, and evaluation for apneic episodes.
Airway-Related Comorbidities
- Current or recent upper respiratory infections (runny nose, cough, sputum, fever, malaise, croup, etc.)
- Sleep-disordered breathing or obstructive sleep apnea (polysomnography or STBUR tool: Snoring, Trouble Breathing, Un-Refreshed in the morning)
- Airway edema (hoarse voice, inspiratory stridor, drooling)
- Asthma and reactive airway disease (frequency of bronchodilator therapy, family or personal history of atopy, grunting during feeds, steroid use)
- Chronic lung disease (oxygen-dependence, recent hospitalizations)
- Exposure to second-hand smoke at home
- Aspiration (history of repeated pneumonias, coughing/gagging with feeds)
- Many pediatric syndromes are known to be associated with a difficult airway (Table 1).3 A high index of suspicion for a difficult airway should be maintained in children with dysmorphic facial features and known syndromic conditions.
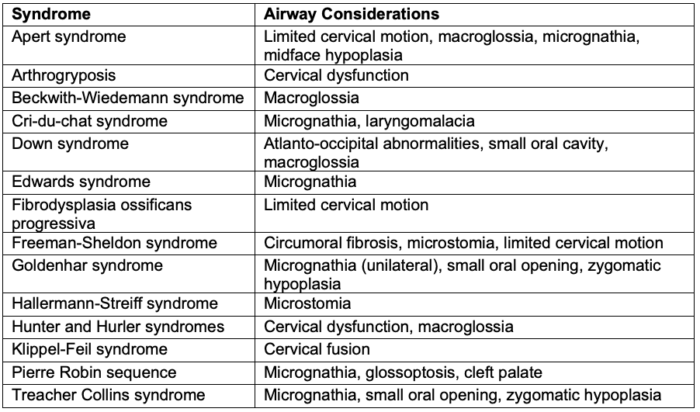
Table 1. Notable pediatric syndromes with airway implications. Adapted from Harless J, et al. Pediatric airway management. Int J Crit Illn Inj Sci. 2014;4(1):65-70.3
Airway Issues During Previous Anesthetics
- Difficult bag-mask ventilation requiring airway adjuncts, significant positive pressure, and/or two-person technique
- History of difficult intubation
- Grade 3 or 4 Cormack and Lehane view on direct laryngoscopy
- Video laryngoscopy view with less than 50% view of vocal cords
- History of multiple (3+) intubation attempts or failed intubation
- It is important to remember that the pediatric airway changes over time and with growth. Therefore, prior uneventful airway management and intubations do not predict the absence of future complications.
Previous Surgical Procedures Involving the Airway
- Airway evaluations (flexible nasopharyngeal laryngoscopy, microlaryngoscopy/ bronchoscopy, drug-induced sleep endoscopy)
- Airway surgeries (supraglottoplasty, balloon dilations for subglottic stenosis, laryngeal papillomas, head and neck radiation, etc.)
Physical Exam
- The physical exam begins with a global physical assessment of the child:
- Vital signs with special attention to respiratory rate and baseline O2 saturation
- Respiratory effort, nasal flaring, presence of retractions (suprasternal, intercostal, or subcostal), and use of accessory muscles
- Adventitious breath sounds, changes in voice/cry, and mentation
- A focused airway exam should also include:
- Evaluation of the mandible, maxilla, and tongue size
- Loose or missing teeth, interincisor distance
- Gross anatomic abnormalities (such as bilateral microtia) or recognizable syndromic features
- Mallampati score, thyromental distance, and upper lip bite test (detailed below)
Mallampati Scoring4
- The original Mallampati scoring system included three classes that was based on the degree that the tongue visually obstructs the oropharynx. It was later expanded to the modified Mallampati scoring system that is in common use today (Figure 1). A Class 0 has been added for visualization of any part of the epiglottis, but this is rarely seen. A higher Mallampati score is suggestive of difficult exposure of the glottis during direct laryngoscopy and, thus increased intubation difficulty.
- The ability to assess the modified Mallampati score and upper lip bite test in pediatric patients will depend on their cooperation with the exam, which serves as a limitation in this population. Mallampati scores of III and IV have been shown to be associated with difficult airway in pediatric patients.5
- Modified Mallampati Classification (Figure 1)
(Patient opens mouth and protrudes the tongue WITHOUT phonation.)
Class I: Visualization of soft palate, uvula, and pillars
Class II: Visualization of soft palate and uvula
Class III: Visualization of soft palate and base of uvula
Class IV: Visualization of only the hard palate, and not the soft palate
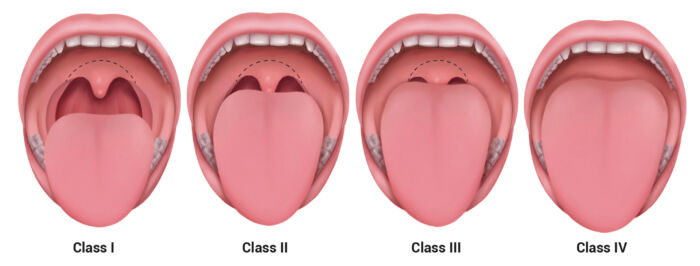
Figure 1. Modified Mallampati classification of oropharyngeal view.
Thyromental Distance6
- Appropriate thyromental distance varies with age and height. An alternate estimate is to evaluate if the distance between the mentum and the neck/mandible junction (near the hyoid bone) is equal to or greater than the width of 3 patient fingers.

Figure 2. Thyromental distance should be at least 3 of the patient’s finger widths, as seen in this 3-year-old child.
Upper Lip Bite Test6
- This test is an additional tool for assessing intubation difficulty that evaluates a patient’s ability to protrude the mandible and is divided into three classes:
- Class I: Lower incisors can bite the upper lip above the vermilion line.
- Class II: Lower incisors can bite the upper lip below the vermilion line.
- Class III: Lower incisors cannot bite the upper lip.
Mnemonic: LEMON Method to Assess Anticipated Airway Difficulty7
- Look Externally: Abnormal Facies? Trauma? Body Habitus? Get a general impression of airway difficulty.
- Evaluate (3-3-2 Rule, which is suggestive of an uncomplicated airway):
- 3: Patient can open their mouth the width of three of their own fingers.
- 3: Distance between the mentum and the neck/mandible junction is the width of three of the patient’s fingers.
- 2: Space between the superior notch of the thyroid cartilage to the neck/mandible junction is the width of two of the patient’s fingers.
- Mallampati score
- Obstruction/Obesity: Supraglottic mass, infection, trauma +/- hematoma, injury with damage to upper airway, redundant tissue, or other mechanical obstruction
- Neck mobility: Assessment may be limited in patients with degenerative joint disease, rheumatoid arthritis, ankylosing spondylitis, etc. Trauma patients requiring in-line stabilization also pose challenges for intubation.
- In summary, the predictors of a pediatric difficult airway include5,8
- Mallampati score of 3 or 4
- Short thyromental distance
- Upper lip bite test class III
- Abnormal face shape
- Midface or mandibular hypoplasia
- Small mouth opening
- Macroglossia
- Bilateral microtia
- Short thyromental distance
- Poor dentition/loose teeth
- Overbite/underbite
- Limited neck range of motion
- Large neck circumference
- A recent multicenter cross-sectional study confirmed the findings of prior studies that suggested that the modified Mallampati test is most predictive of difficult laryngoscopy, followed by the upper lip bite test and thyromental distance.8
Diagnostic Studies1
- Preoperative airway diagnostic studies should be obtained only on an as-needed basis with appropriate clinical reasoning and options include:
- Radiographic imaging
- Endoscopy
- Lung function tests
- Polysomnography
- Radiographic imaging may provide further noninvasive data, though care should be taken to minimize radiation exposure. Common modalities include neck and chest x-rays, computed tomography, and magnetic resonance imaging.
- In a patient with a compromised airway, radiographic imaging should only be performed in the presence of qualified personnel and difficult airway equipment.
- Flexible fiberoptic endoscopy at the bedside allows direct visualization of the airway, mobility of the vocal cords, dynamic airway compression, etc.
- A sleep study or polysomnography may be used to further assess patients with snoring, upper airway resistance, and suspected obstructive hypopnea and apnea.
- Lung function tests such as spirometry, pulmonary function tests, capillary blood and arterial blood gas sampling may be considered in patients with advanced pulmonary disease.
- Laboratory data such as hypo/hyperthermia, abnormal clotting, abnormal acid-base balance, and electrolyte derangements should be considered when determining the approach to induction and intubation.
References
- Adewale L. Anatomy and assessment of the pediatric airway. Pediatr Anesth. 2009; 19:1-8. PubMed
- Wheeler DS, Spaeth JP, Mehta R, et al. Assessment and management of the pediatric airway. In: Wheeler D, Wong H, Shanley T. (eds) Resuscitation and Stabilization of the Critically Ill Child. London; Springer; 2009.
- Harless J, Ramaiah R, Bhananker SM. Pediatric airway management. Int J Crit Illn Inj Sci. 2014; 4(1):65-70. PubMed
- Stutz EW, Rondeau B. Mallampati Score. In: StatPearls [Internet]. Treasure Island (FL); StatPearls Publishing; 2022. StatPearls
- Santos AP, Mathias LA, Gozzani JL, et al. Difficult intubation in children: applicability of the Mallampati index. Rev Bras Anestesiol. 2011; 61(2):156-8, 159-62, 84-7. PubMed
- Khan ZH, Mohammadi M, Rasouli MR., et al. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: A prospective study. Anesth Analg. 2009; 109(3):822-4. PubMed
- Reed MJ, Dunn MJ, McKeown DW. Can an airway assessment score predict difficulty at intubation in the emergency department? Emerg Med J. 2005; 22(2):99-102. PubMed
- Sitot M, Amare W, Aregawi A. Predictive values of the modified Mallampati test, upper lip bite test, thyromental distance and ratio of height to thyromental distance to predict difficult laryngoscopy in pediatric elective surgical patients 5-12 years old at selected Addis Ababa governmental hospitals, Ethiopa: a multicenter cross-sectional study. BMC Anesthesiol. 2022; 22:364. PubMed
Other References
- Basic Pediatric Airway Anatomy and Assessment. The Children’s Hospital of Philadelphia Pediatric Airway Skills Education Program. Accessed 01/10/2023. Link
- Liston DE, Hunyady A, Karl HW. Pediatric airway management for the non-anesthesiology. Society for Pediatric Anesthesia Global Lecture Series. Accessed 01/10/23. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.