Copy link
Optimizing Pediatric Intubation
Last updated: 01/20/2023
Key Points
- An airway management plan should be simple and clear, with a detailed understanding of all possible complications and how to manage them before initiating the plan.
- Optimizing pediatric tracheal intubation requires managing three crucial “arms” to maintain safety during the attempt: oxygenation, maintenance of anesthetic/sedation depth, and proper selection and use of devices and techniques based on the existing airway problem.
- Passive oxygenation throughout tracheal intubation can provide greater apnea tolerance.
- Adequate anesthetic/sedation depth will optimize tracheal intubation conditions and reduce tracheal intubation-related complications.
Introduction
- Tracheal intubation failure in children can lead to critical events, including life-threatening hypoxemia and cardiac arrest. Infants and small children are at a higher risk for difficult tracheal intubation and related complications.1,2
- In the first report from the Pediatric Difficult Intubation (PeDI) registry, more than two tracheal intubation attempts, a weight less than 10kg, short thyromental distance, and three direct laryngoscopy attempts before an indirect technique were associated with an increased risk of complications.1
- More recently, a secondary analysis of tracheal intubations of the Neonate and Children audit of Anaesthesia pRactice IN Europe (NECTARINE) trial found a high incidence (5.8%) of difficult tracheal intubations (defined as more than two direct laryngoscopy attempts) in children younger than 60-weeks postconceptual age resulting in severe hypoxemia (SpO2 <90% for 60 seconds) in 40% of patients.3
- Therefore, every neonatal tracheal intubation should be considered a critical event.4 We should optimize the conditions for first attempt tracheal intubation success without adverse effects in this vulnerable population.
- Team dynamics, delegation of roles, checklists, time-outs, backup plans/personnel, and other human factors play an important role.4 Airway management is not limited to choosing the right device for airway instrumentation and being proficient in its use, but also includes other essential components of airway management such as oxygenation and maintenance of adequate anesthetic depth.4
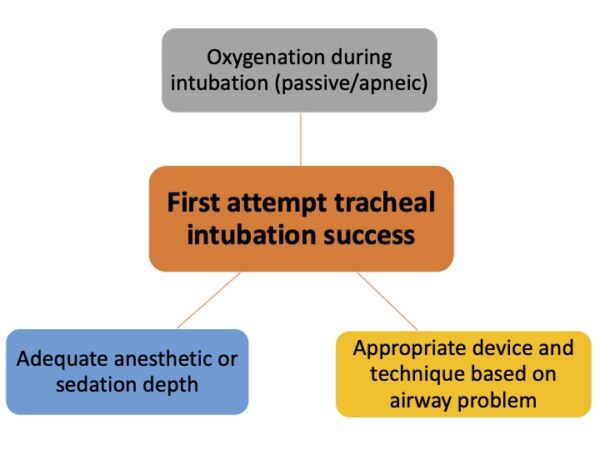
Figure 1. Three pillars of successful airway management in children. Adapted from: Garcia-Marcinikiewicz AG, Matava CT. Safe in the first attempt: teaching neonatal airway management. Curr Opin Anaesthesiol. 2022;35(3): 329-36.4
Passive Oxygenation
- Hypoxemia related to tracheal intubation is an important cause of morbidity and mortality in children.3,5 Reduced functional residual volume and increased oxygen consumption make small children and neonates prone to hypoxemia during laryngoscopy.
- Supplemental oxygenation is an important factor in optimizing tracheal intubation and its safety.
- Providing passive oxygenation increases the apnea tolerance time during intubation, potentially leading to a calmer, less hurried, and less traumatic intubation.5
- In a study involving young children undergoing general anesthesia requiring tracheal intubation for elective surgery, conventional low-flow oxygen (100% oxygen at 0.2 L/kg/min) and transnasal humidified rapid insufflation ventilator exchange (THRIVE) 100% oxygen, significantly prolonged apnea time with no significant difference between the two techniques.6
- A recent randomized controlled trial found that among infants undergoing endotracheal intubation, nasal high-flow oxygen during the procedure improved the likelihood of successful intubation on the first attempt.7
- There are several methods of providing supplemental oxygen, including conventional nasal cannula, modified nasopharyngeal airway, and a swivel adapter connecting the supraglottic airway device to the anesthesia machine circuit are some examples (Figure 2). Delivering oxygen should not obstruct the view of the laryngoscopist, and it should be delivered through a patent airway.
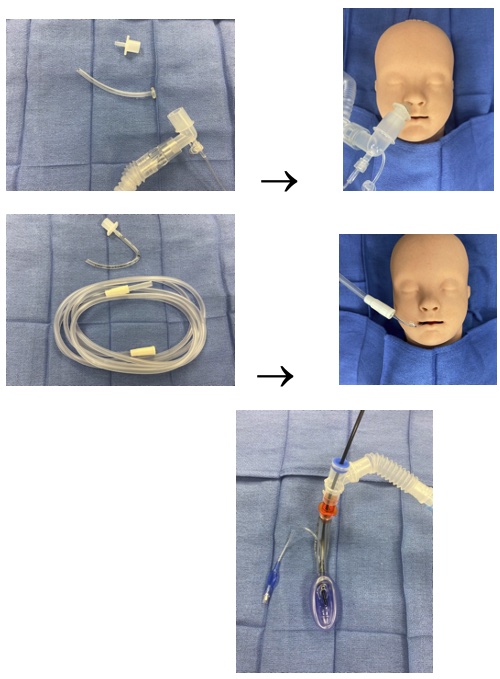
Figure 2. Methods of providing supplemental oxygen. A-oxygen insufflation via a nasopharyngeal airway with a 15mm tube connector. B-oxygen insufflation via a RAE tube and suction tubing inserted as a hook into the patient’s mouth. C-oxygen insufflation during a fiberoptic intubation through a supraglottic airway using a swivel adapter. Adapted from: Garcia-Marcinikiewicz AG, Matava CT. Safe in the first attempt: teaching neonatal airway management. Curr Opin Anaesthesiol. 2022;35(3): 329-36.4
Proper Anesthetic Depth
- Ideally, we would have all the time required to carefully intubate a patient with no motor or airway reflexes in response to intubation. However, this is not a realistic expectation.4
- Adequate anesthetic depth matters and is required to prevent adverse events such as laryngospasm and improve tracheal intubation success. The choice of anesthetic technique and sedation depends on the patient’s anatomic and physiologic circumstances.4
- To paralyze or not to paralyze is an important decision that must be made prior to tracheal intubation.
- Whether neuromuscular blocking drugs (NMBD) are given or not, appropriate anesthetic depth must be maintained throughout the intubation attempt to avoid airway-related complications.
- A recent randomized controlled trial in which infants were allocated to high-flow oxygen vs. conventional therapy also noted that across both groups, the first attempt tracheal intubation success was lower when NMBD was not given.7
- Another study from the PeDI registry found that spontaneous ventilation is associated with more nonsevere complications, such as hypoxemia and laryngospasm, compared to controlled-ventilation techniques.8
- A study involving ten neonatal ICUs found that tracheal intubation-associated complications were higher when NMBD was not used.9
- A more recent PeDI study found that 27% of sedated tracheal intubation attempts in children with difficult airways needed to be converted to general anesthesia for successful tracheal intubation.10
Appropriate Devices
- Commonly used methods for endotracheal intubation are direct laryngoscopy, video laryngoscopy, and fiberoptic intubation.
- Choosing the appropriate device in the appropriate size is key. From standard direct laryngoscopy blades (Miller and Macintosh) to standard and nonstandard hyperangulated video laryngoscopes and fiberoptic scopes, the designs of airway devices have evolved to provide a range of sizes tailored to the specific anatomic needs of neonates and infants.
- It is important to choose the right equipment depending on the type of airway anticipated. For example, in a patient with severe micrognathia, a hyperangulated blade or fiberoptic intubation through a supraglottic device may assist with the “very acute” angle to the airway, with the added benefit of passive oxygenation/ventilation through the supraglottic device.4
- The video laryngoscopy in small infants (VISI) trial reported improved first-attempt success rate and reduced complications among anesthetized infants using video laryngoscopy with a standard blade.11
References
- Fiadjoe JE, Nishisaki A, Jagannathan N, et al. Airway management complications in children with difficult tracheal intubation from the Peditriac Difficult Intubation (PeDI) registry: a prospective cohort analysis. Lancet Respir Med. 2016; 4(1): 37-48. PubMed
- Disma N, Leva B, Dowell J, et al. Assessing anaesthesia practice in the vulnerable age group: NECTARINE: A European prospective multicentre observational study. Eur J Anaesthesiol. 2016; 33(4):233-35. PubMed
- Disma N, Virag K, Riva T, et al. Difficult tracheal intubation in neonates and infants. NEonate and Children audiT of Anaesthesia pRactice IN Europe (NECTARINE): a prospective European multicentre observational study. Br J Anaesth. 2021.126(6): 1173-81. PubMed
- Garcia-Marcinikiewicz AG, Matava CT. Safe in the first attempt: teaching neonatal airway management. Curr Opin Anaesthesiol. 2022;35(3): 329-36. PubMed
- Fiadjoe JE, Litman RS. Oxygen supplementation during prolonged tracheal intubation should be the standard of care. Br J Anaesth. 2016;117(4):417-18. PubMed
- Riva T, Pedersen TH, Seiler S, et al. Transnasal humidified rapid insufflation ventilatory exchange for oxygenation of children during apnoea: a prospective randomised controlled trial. Br J Anaesth. 2018;120(3):592-99. PubMed
- Hodgson KA, Owen LS, Kamlin COF, et al. Nasal High-Flow Therapy during Neonatal Endotracheal Intubation. N Engl J Med. 2022;386(17):1627-37. PubMed
- Garcia-Marcinkiewicz AG, Adams HD, Gurnaney H, et al. A Retrospective Analysis of Neuromuscular Blocking Drug Use and Ventilation Technique on Complications in the Pediatric Difficult Intubation Registry Using Propensity Score Matching. Anesth Analg. 2020;131(2):469-79. PubMed
- Foglia EE, Ades A, Sawyer T, et al. Neonatal Intubation Practice and Outcomes: An International Registry Study. Pediatrics. 2019;143(1). PubMed
- Sequera-Ramos L, Laverriere EK, Garcia-Marcinkiewicz AG, et al. "Sedation versus General Anesthesia For Tracheal Intubation In Children With Difficult Airways: A Cohort Study from the Pediatric Difficult Intubation Registry.". Anesthesiology. 2022. PubMed
- Garcia-Marcinkiewicz AG, Kovatsis PG, Hunyady AI, et al. First-attempt success rate of video laryngoscopy in small infants (VISI): a multicentre, randomised controlled trial. Lancet. 2020;396(10266):1905-13. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.