Copy link
Obstructive Sleep Apnea: Pathophysiology
Last updated: 05/24/2024
Key Points
- Obstructive sleep apnea (OSA) results in repetitive narrowing and collapse of the pharyngeal airway due to reduced pharyngeal muscle tone during sleep.
- Contributory factors include an unfavorable upper airway anatomy, low respiratory arousal threshold, high loop gain, and poor muscle responsiveness.
- Wide variations in the estimates of prevalence are seen that are related to the overlap of various pathophysiological phenotypes and endotypes.
Definition
- Obstructive sleep apnea (OSA) is characterized by recurrent episodes of apnea or hypopnea during sleep, resulting in varying severity of hypoxemia, hypercapnia, and frequent cortical arousals from sleep.1
- It results from the repetitive narrowing and partial or complete collapse of the pharyngeal airway due to an exaggerated reduction in pharyngeal muscle tone.
Epidemiology
- Estimates of the prevalence of OSA show a wide variation.
- The Wisconsin Sleep Cohort Study estimated that mild OSA was present in 33.9% of men and 17.4% of women in the United States, while moderate or severe OSA was present in 13% of men and 5.6% of women.1
- The prevalence of OSA increases with advancing age, increased body mass index, and male sex. OSA is approximately twice as common in men as in women.1
- Patients undergoing bariatric surgery may have a prevalence of up to 70%.
- Approximately 60-90% of patients with moderate to severe OSA may remain undiagnosed in the perioperative period.
Pathophysiology and Phenotypes
- Upper airway dilator muscles (genioglossus, levator palatini, tensor palatini, geniohyoid, and stylopharyngeus) are responsible for maintaining airway patency during inspiration.
- The genioglossus is the most important upper airway dilator muscle that contracts with each inspiration to prevent the posterior collapse of the tongue. It is assisted by the levator and tenso palatini muscles, which advance and elevate the soft palate, and the geniohyoid and stylopharyngeus muscles which prevent the medial collapse of the lateral pharyngeal walls.1
- Reduction in dilator muscle activity during sleep leads to airway collapse.1
- Narrowing of the upper airway is common in patients with OSA. This can result from an elongated soft palate, increased tongue fat and inferior hyoid position, fat deposition in the lateral pharyngeal wall, or from skeletal features including mandibular retrognathia and a shorter mandibular or maxillary length1 (Figure 1).
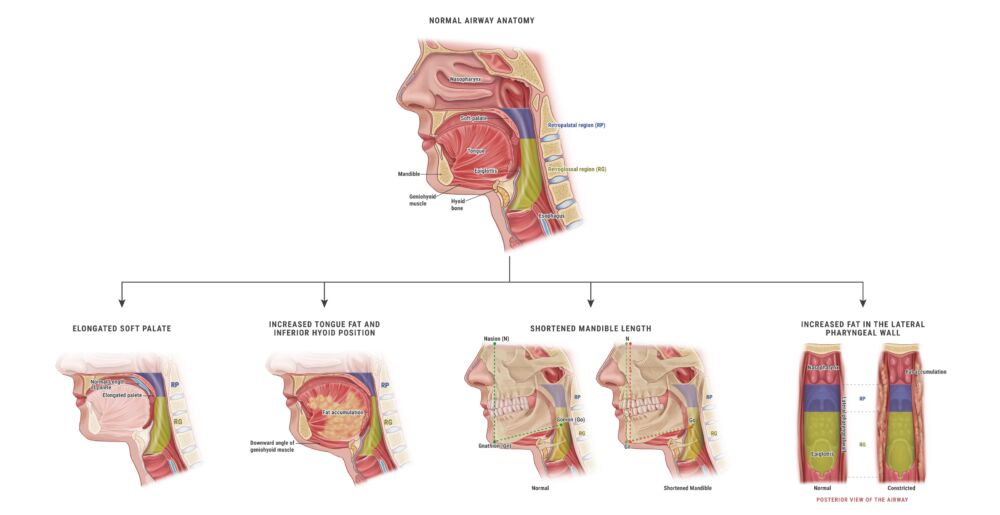
Figure 1. Anatomical features of OSA. Redrawn from Gottlieb DJ, Punjabi NM. Diagnosis and management of obstructive sleep apnea. A review. JAMA. 2020; 323(14): 1380-1400.
- Airway collapse results in apnea or hypopnea despite adequate respiratory efforts. This leads to large swings in intrathoracic pressure with intermittent hypoxemia, hypercapnia, and arousals from sleep.
- Hypoxemia and hypercapnia result in sympathetic activation and elevated blood pressures.
- Elevated catecholamines also blunt insulin sensitivity, which may contribute to the increased risk of diabetes mellitus.
- Other contributory factors include an impaired mechanoreceptor response to intrapharyngeal pressures, ventilatory overshoot, and an increased arousal threshold.2
Endotypes of OSA
- To address the complex pathophysiology of OSA, phenotypes and endotypes of OSA have been developed.2
- Phenotype refers to the observable expressions of individual characteristics that result from interactions of genetic material and the environment.
- Endotype refers to a disease subtype defined by a distinct pathophysiologic mechanism.
- A specific phenotype may include several endotypes.
- Endotypes of OSA can be classified into anatomical and physiological endotypes.
Anatomical Endotypes: Obesity and Craniofacial Morphology
- Obesity and upper airway collapsibility are important determinants of the severity of OSA.2
- Obesity
- Obesity is the most common risk factor for OSA. The pattern of fat distribution (neck and waistline) is more important than the overall weight.
- Neck circumference is a strong predictor for sleep-disordered breathing with fat deposition in the parapharyngeal areas resulting in OSA.
- Android pattern of fat deposition in the abdomen, especially in men, reduces lung volumes and causes traction on the pharynx, increasing pharyngeal collapsibility.
- Fortunately, obesity is a modifiable risk factor. Reduction in weight through diet, exercise, and bariatric surgery is associated with an improvement in OSA severity.
- Craniofacial morphology
- Craniofacial morphology is another anatomical risk factor. Characteristics associated with OSA include inferiorly placed hyoid, retrognathia, smaller cranial base, and abnormal upper airway soft tissue morphology.2
- Targeted treatments for craniofacial characteristics include mandibular advancement, tongue retaining splints, uvulopalatopharyngoplasty, etc.
Physiological Endotypes
- Several physiological endotypes have been proposed.
Reduced Upper Airway Dilator Muscle Tone
- Reduced tone of the upper airway dilator muscles, especially the genioglossus, contributes to OSA. The genioglossus pulls the base of the tongue anteriorly, off the posterior pharyngeal wall. It normally responds to hypoxia, hypercapnia and increased negative intrathoracic pressures.
- In OSA patients, electromyographic activity of the genioglossus muscles is greater during wakefulness but reduced during sleep, especially during rapid eye movement (REM) sleep as compared to non-REM (NREM) sleep.
- Hypoglossal nerve stimulation is a useful modality to improve airway patency.
Altered Respiratory Arousal Threshold
- Patients with OSA can have either a high or low respiratory arousal threshold, which is defined as the ease at which a sleeping person can be awakened.
- At present, it is difficult to differentiate between the two preoperatively.
- Low arousal threshold disrupts sleep architecture. Sudden arousals lead to rapid respiratory neuronal activity with resultant hyperventilation. This leads to a quick decrease in carbon dioxide to below the apneic threshold, which can lead to a central apnea. Hypocapnia can also further destabilize ventilatory control.
- Patients with low arousal thresholds are more likely to have mild-to-moderate OSA with relatively more hypopnea events, as compared to apneas. They may benefit from sedative agents, such as eszopiclone and trazadone, that improve sleep quality.
- Patients with high arousal threshold have a lower propensity to wake up from sleep and are predominantly associated with severe OSA. These patients are at a higher risk of adverse respiratory events with opioid use, which is especially important in the perioperative period. Opioids both reduce respiratory neuronal activity and impair arousal in response to hypoxia. Sedatives and hypnotics place these patients at particularly high risk of postoperative respiratory depression and morbidity.
Ventilatory Control Stability
- Instability in ventilatory control is a major contributor to OSA. An increase in ventilatory drive activates the upper airway muscles and promotes patency, while a decrease in ventilatory drive relaxes the upper airway muscles and promotes airway closure.2
- Loop gain describes the stability of a feedback response system. For ventilatory control, it is described as the ratio of the ventilatory response to the disturbance. When the loop gain is less than 1, the system is inherently stable, while a loop gain of 1 or greater is unstable.
- High loop gain indicates increased sensitivity of the system to hypoxia and hypercapnia. An increased response to arousal may lead to hypocapnia and reduced ventilatory drive, precipitating central apneas.
- Oxygen has been shown to help reduce loop gain through reducing the response of peripheral chemoreceptors to hypoxia and hypercapnia.
- However, it is difficult to measure loop gain clinically.
Fluid Retention and Rostral Fluid Shift
- OSA is more common in patients with congestive heart failure and end-stage renal failure conditions characterized by intravascular and interstitial fluid retention. It is hypothesized that a redistribution of this fluid may occur on lying down at night. Some fluid may also accumulate in the neck, narrowing the upper airway. Further work is needed to elucidate this mechanism’s role in the perioperative period.
Phenotypes of OSA
- There are several clinical phenotypes of OSA based on age, sex, ethnicity, REM sleep, and supine position2 (Table 1 and Figure 2).
OSA and Age
- The incidence of OSA increases with age, reaching a plateau at around 65 years of age.
- Increased parapharyngeal fat deposition predisposes elderly individuals to OSA.
- Overnight rostral fluid shifts, higher surface tension of the upper airway, and decreased lung volume tethering contribute to airway collapsibility in the elderly.
- Younger patients are more likely to have a higher loop gain, with prominent daytime sleepiness.
OSA and Sex
- Males are 2-3 times more likely to have OSA than females.
- Men have longer apneic events and more significant episodes of oxygen desaturation.
- Anatomic features are contributory with more fat deposition around the upper airway.
- An android pattern of fat deposition contributes to reduced lung volume and increased upper airway collapsibility.
OSA and Ethnicity
- Relative importance of contributory anatomic features varies across ethnicities.
- Asian OSA populations display more craniofacial skeletal restriction.
- African Americans display more obesity and enlarged upper airway soft tissue.
- Caucasians have contributions from both bony and soft tissue abnormalities.
OSA in REM Sleep
- Apneic and hypopneic events are longer and more severe in REM sleep.
- REM sleep is associated with hypotonia and reduced responsiveness of the genioglossus muscle to negative intrapharyngeal pressures.
- Treatment targeting genioglossus tone may reduce obstructive events in REM-related OSA.
Supine Position-Related OSA
- Supine position related OSA can be attributed to unfavorable upper airway anatomy, reduced lung volume and ineffective dilator muscle activity.
- Patients with supine position-related OSA are more likely to be subjectively sleepier than patients with other phenotypes.
- Recognition of this phenotype is clinically useful as these patients are more likely to benefit from positional therapy and oral appliances.
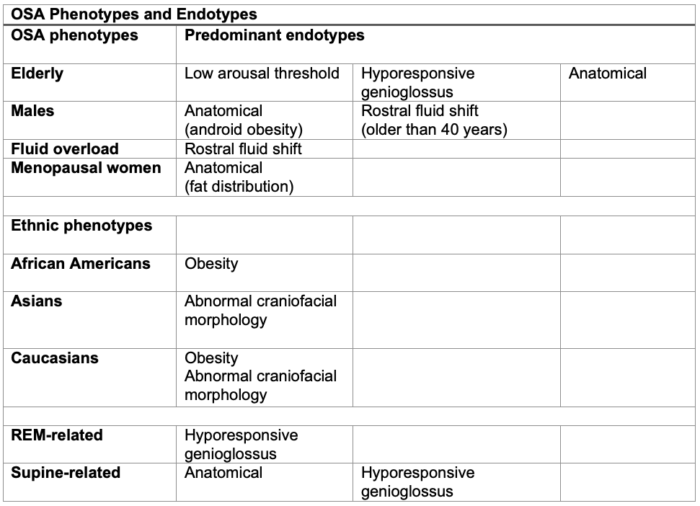
Table 1. OSA phenotypes and endotypes. Adapted from Subramani Y, et al. Understanding phenotypes of obstructive sleep apnea: Application in anesthesia, surgery, and perioperative medicine. Anesth Analg. 2017.2
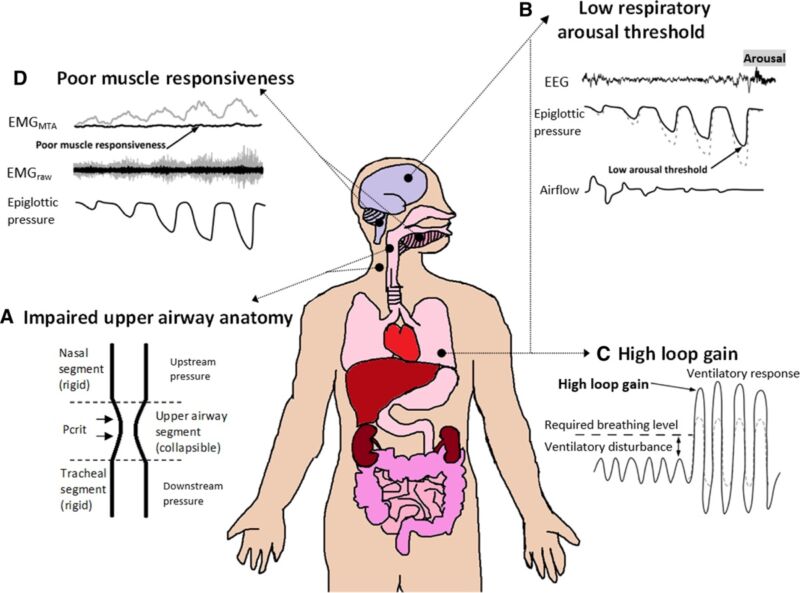
Figure 2. Schematic of the four key phenotypes that contribute to OSA pathogenesis. Used with permission from Altree TJ, et al. Vulnerability to postoperative complications in obstructive sleep apnea: Importance of phenotypes. Anesth Analg. 2021; 1328-37.3
References
- Gottlieb DJ, Punjabi NM. Diagnosis and management of obstructive sleep apnea. A review. JAMA. 2020; 323(14): 1380-1400. PubMed
- Subramani Y, Singh M, Wong J, et al. Understanding phenotypes of obstructive sleep apnea: Applications in anesthesia, surgery, and perioperative medicine. Anesth Analg. 2017; 124(1): 179-91. PubMed
- Altree TJ, Chung F, Chan MTV, et al. Vulnerability to postoperative complications in obstructive sleep apnea: Importance of phenotypes. Anesth Analg. 2021; 1328-37. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.