Copy link
Massive Hemorrhage Protocol
Last updated: 09/06/2024
Key Points
- Massive hemorrhage (MH) can be defined based on volume lost or volume administered.
- Protocols: A Massive Transfusion Protocol (MTP) ensures rapid blood component delivery and administration. A Massive Hemorrhage Protocol (MHP) integrates an MTP and additional critical aspects of care, including mitigating complications from bleeding and/or transfusion.
- Blood components vs. products: Blood components (RBCs, plasma, platelets, cryoprecipitate) are separated from whole blood, while blood products include any therapeutic substance derived from human blood (e.g., fibrinogen concentrate) or are genetically engineered.
Introduction
MH Definitions
- Several definitions have been used to define MH and massive transfusion (MT).
- Based on volume lost, MH has been defined as:
- Loss of greater than one blood volume (BV) in 24 hours,
- 50% of BV lost in 3 hours, or
- greater than 10% of BV lost every 10 minutes.
- Historically, MT was defined as the transfusion of ten or more units of whole blood or RBCs in 24 hours. Ultra-massive transfusion has been defined as using 20 or more units in 24 or 48 hours.
- Critical administration threshold for 1 hour (CAT-1) is an alternative functional definition involving administering three or more units of RBCs or whole blood over one hour.1
- The Resuscitation Intensity (RI) score is similar to CAT but uses four or more blood components (all blood products and fluids) in 30 minutes as a starting point.1
- In children, MT is defined as:
- More than 40 mL/kg total components in 24 hours (combat trauma) or
- More than 40 mL/kg total components or 20 mL/kg RBC over 4-6 hours (civilian trauma).2
- Etiology: Trauma causes 50% of MTP activations; firearms are now the leading cause of child death in the United States. Medical and surgical bleeding evenly account for the other 50% of MTP activations.
- Adult and pediatric MH mortality: About two-thirds of deaths due to traumatic hemorrhage occur in the first 6 hrs.
- Pediatric MH 28-day mortality: Highest in medical patients (65%), then trauma (36%) and surgery (24%).3 In trauma, more than 50% of mortality occurs due to central nervous system injury.
- The benefits of MTP implementation: Unlike adults, MTP has not improved 30-day mortality rates in children, which are 2-3 times higher (35.3-47.1%) due to their unique size, anatomy, physiology, and increased risk for adverse transfusion events.
MHP Activation and Patient Management
- Key protocol elements (see Table 1 below) should be adapted to local resources.
- Ensure clear communication of activation/deactivation, critical lab results, patient location changes, and use of patient hand-over tools.
- Emphasize early strategies to STOP bleeding.
- Plan a rapid transition from ratio-based to goal-directed transfusion; consider whole blood.
- There is no specific threshold at which cross-matched RBCs should be avoided based on the number (or volume) of uncross-matched O-negative RBC units administered. Transition as soon as possible to cross-matched PRBCs.
- Utilize blood conservation strategies (e.g., restrictive transfusion thresholds, tranexamic acid, and autologous red blood cell scavenging).
- Mitigate/treat complications from massive hemorrhage or transfusion, including metabolic derangements (e.g., ↑ K+, ↓ Ca2+), acidosis, coagulopathy, and hypothermia.
- Ensure regular practice audits and continuous quality improvement.
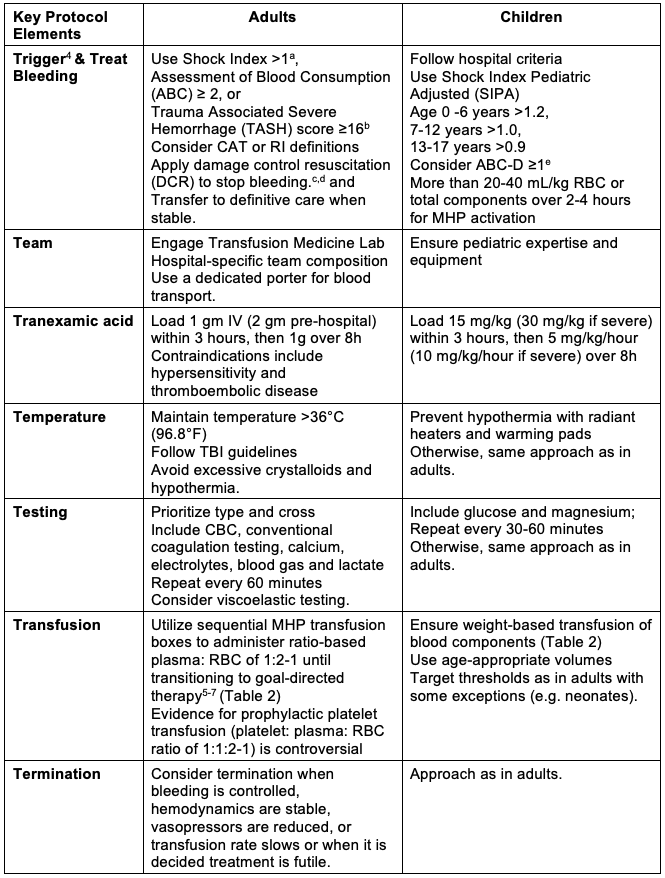
Table 1. The key “7 Ts” elements of a massive hemorrhage protocol. Modified with permission from Tan GM et al. Pediatr Anesth. 2023; 33: 609-19.
Table 1 (cont.)
aShock index is the heart rate divided by systolic blood pressure. A normal shock index is 0.5-0.7. In trauma patients, a shock index greater than 0.9 is associated with an increased risk of transfusion and mortality.
bThere are several validated scores to predict massive transfusion in adult trauma patients.4 The ABC score is based on four clinical criteria, each weighted at one point.
- Penetrating mechanism of injury
- Positive abdominal FAST (Focused Assessment with Sonography for Trauma)
- Systolic blood pressure ≤ 90 mmHg and
- Heart rate ≥ 120 beats/minute).
The TASH score is calculated using multiple clinical and laboratory variables, and each variable is assigned a certain number of points based on its association with severe hemorrhage.
- Systolic blood pressure
- Hemoglobin level
- Positive abdominal FAST
- Heart rate
- Gender
- Pelvic fracture and complex long bone fractures
cDamage control resuscitation (DCR) aims to avoid the lethal triad of hypothermia, acidosis, and coagulopathy. The fundamental tenets of DCR include
- Control hemorrhage
- Avoid hypotension
- Ensure adequate oxygen delivery
- Limit crystalloids
- Administer warmed blood components and
- Quickly progress from ratio-based to laboratory-guided (goal-directed) hemostatic resuscitation.
dMeasures to STOP bleeding include
- Surgery (vessel ligation, damage control laparotomy, packing, and direct pressure),
- Mechanical (tourniquets/pelvic binder, hemostatic gauze, balloon tamponade for gastrointestinal bleeding),
- Endovascular technique (radiologic embolization or stenting) and
- Topical hemostatic agents (e.g., gelatin sponge).
eABC-D tool is similar to the adult ABC tool but replaces the heart rate and blood pressure thresholds with an age-appropriate shock index pediatric adjusted (SIPA) and incorporates measures of inadequate oxygen delivery (base deficit > – 8.8 and lactate >3.5 mmol/L)
Abbreviations: CBC=complete blood count (hemoglobin, white blood cell, and platelet count); CHD=congenital heart disease; CAT=critical administration threshold; RI=resuscitation intensity; MHP=Massive Hemorrhage Protocol; RBCs=red blood cells; TXA=tranexamic acid; TBI=traumatic brain injury; QI=quality indicator.
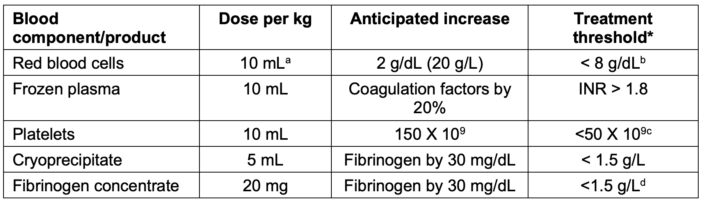
Table 2. Pediatric dosing and therapeutic targets for blood components/products. Adapted with permission Tan GM, et al. Pediatr Anesth. 2023; 33: 609-19.
Treatment thresholds are similar between adults and children. Some exceptions are described below.
a. In the setting of massive hemorrhage, the anticipated rise in hemoglobin may be less than expected, requiring a 20 mL/kg dose of RBCs.
b. Higher hemoglobin treatment thresholds may be required for some comorbidities (e.g., cyanotic heart disease or traumatic brain injury) and age (e.g., premature infant).
c. An intracranial hemorrhage may require a higher platelet treatment threshold (<100 × 109).
d. In cardiac surgery, a higher fibrinogen dose (70 mg/kg, maximum 4 g or 2 g if less than 30 kg) and treatment threshold (less than 2.0 g/L) may be required.
Please see Figure 1 for a summary of pediatric massive hemorrhage guidelines.
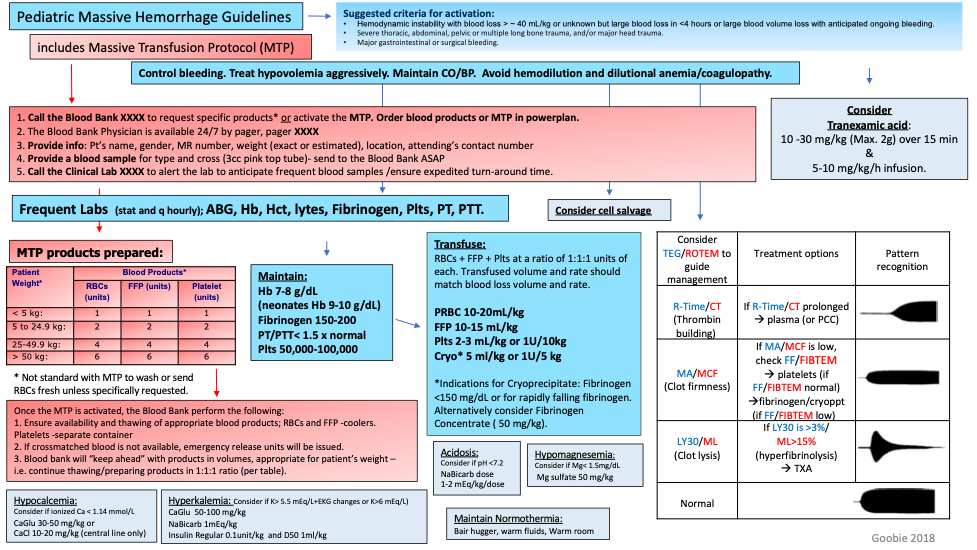
Figure 1. Summary of pediatric massive hemorrhage guidelines. Used with permission from Goobie SM, et al. Society for the advancement of blood management administrative and clinical standards for patient blood management programs. 4th edition (pediatric version). Paediatr Anaesth. 2019;29(3): 231-6.10
Monitoring of Massive Transfusion
- Monitor shock severity and resuscitation response: Regularly check cardiovascular (pulses, heart rate, blood pressure), integumentary (capillary refill), respiratory (rate and depth), central nervous system (mental status, Glasgow coma scale, temperature), and renal (urine output) organ systems.
- Class II to class III shock transition: This transition indicates a failure of compensatory mechanisms, which is often masked in children due to their strong cardiovascular response.
- Blood, the body’s largest organ, is composed of cells, plasma, and vascular endothelium. It can fail due to hemorrhagic shock and is modulated by tissue injury.
- Blood failure is an emergency characterized by critical oxygen debt (shock), with evidence of low tissue oxygen delivery, endotheliopathy, platelet dysfunction, and coagulopathy.8
- Monitor blood failure: Use hemoglobin, lactate, pH, base deficit, and coagulation tests.9
- Viscoelastic testing in children is often underutilized due to cost and limited data on normal values and outcomes.
References
- Meyer DE, Cotton BA, Fox EE, et al. A comparison of resuscitation intensity and critical administration threshold in predicting early mortality among bleeding patients: A multicenter validation in 680 major transfusion patients. J Trauma Acute Care Surg. 2018;85(4):691. PubMed
- Rosenfeld E, Lau P, Zhang W, et al. Defining massive transfusion in civilian pediatric trauma. J Pediatr Surg. 2019;54(5):975-9. PubMed
- Leonard JC, Josephson CD, Luther JF, et al. Life-threatening bleeding in children: A prospective observational study. Crit Care Med. 2021;49(11):1943-54. PubMed
- Gianola S, Castellini G, Biffi A, et al. Accuracy of risk tools to predict critical bleeding in major trauma. A systematic review with meta-analysis. J Trauma Acute Care Surg. 2022;92:1086-96. PubMed
- Cardenas JC, Zhang X, Fox EE, et al. Platelet transfusions improve hemostasis and survival in a substudy of the prospective, randomized PROPPR trial. Blood Adv. 2018;2:1696-1704. PubMed
- Holcomb JB, Tilley BC, Baraniulk S, et al. Tranfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma; the PROPPR randomized clinical trial. JAMA. 2015;313:471-82. PubMed
- Nguyen M, Pirrachio R, Kornblith LZ, et al. Dynamic impact of transfusion ratios on outcomes in severely injured patients. Targeted machine learning analysis of the PROPPR randomized clinical trial. J Trauma Acute Care Surg. 2020;89:5105-13. PubMed
- White NJ, Ward KR, Pati S, Strandenes G, Cap AP. Hemorrhagic blood failure: Oxygen debt, coagulopathy, and endothelial damage. J Trauma Acute Care Surg. 2017;82 (6S Suppl):S41-S49. PubMed
- Tan GM, Murto K, Downey LA, et al. Error traps in Pediatric Patient Blood Management in the Perioperative Period. Paediatr Anaesth. 2023;33:609-19. PubMed
- Goobie SM, Gallagher T, Gross I, et al. Society for the advancement of blood management administrative and clinical standards for patient blood management programs. 4th edition (pediatric version). Paediatr Anaesth. 2019;29(3): 231-6. PubMed
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.