Copy link
Liver Disease Scoring Systems
Last updated: 08/02/2024
Key Points
- Using unbiased scoring systems allows for the objective selection of recipients for liver transplantation (LT).
- Scoring systems have evolved using the best evidence to improve predictability.
- The Child-Turcotte-Pugh (CPT), Model for End-Stage Liver Disease (MELD), and Pediatric Model for End-Stage Liver Disease (PELD) scoring systems (and versions thereof) are commonly used and easily accessible.
Introduction
- Scoring systems for the severity of liver disease were developed to predict mortality and help decide on the urgency for LT.
- Over time, they have evolved with ever-increasing accuracy due to increased experience with data and the use of objective variables.
- The position that a patient occupies on the waiting list for LT depends on the score assigned to them using regular monitoring of blood test results.
- In the US, the National Organ Transplant Act established the Organ Procurement and Transplantation Network (OPTN) to allow for more equitable organ allocation and access for patients needing transplantation.
- OPTN: a public-private partnership that oversees the organ transplantation system and links transplant centers and professionals.
- UNOS (United Network for Organ Sharing): a private, nonprofit organization that administers the OPTN under federal contract.
CTP Score Link
- The score was originally designed in 1964 by Drs. Child and Turcotte to guide the selection of patients with cirrhosis who may benefit from portal decompression via a portal shunt placement.1
- In 1972, Pugh et al. modified the CTP score by replacing nutritional status with the more objective measurement of prothrombin time (PT).
- Later, it was successfully validated as an instrument for evaluating both short- and long-term prognosis in patients with cirrhosis.
- It was used as a tool to guide organ allocation from 1998-2002 and currently incorporates five parameters (serum albumin, serum bilirubin, prothrombin time, degree of encephalopathy, and severity of ascites) to group patients into three increasing levels of disease severity: A, B or C (Table 1).
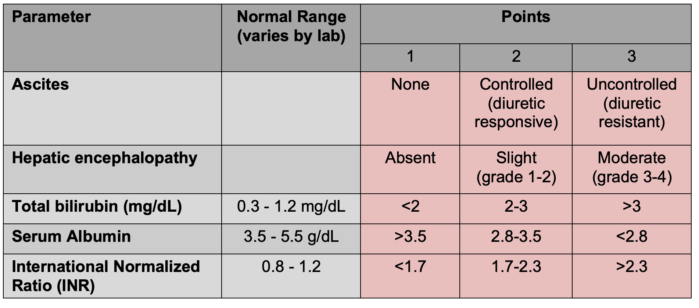
Table 1. Child-Turcotte-Pugh classification for the severity of cirrhosis is obtained by adding up the scores for each parameter. Class A (least severe liver disease) = 5-6 pts; Class B (moderately severe liver disease) = 7-9 pts; Class C (most severe liver disease) = 10-15 pts. Alternative descriptions of the three classes include well compensated, functionally compromised, and decompensated as severity increases. In addition, it has been used to predict mortality risk in major operations: after open abdominal surgery, Class A=10% mortality, Class B=30% mortality, and Class C=70-80% mortality.
- The disadvantages of the CPT score include the subjective assessment of ascites and hepatic encephalopathy and the lack of validation in other patient demographic or disease severity groupings.
MELD Score Link
MELD = 3.8*loge(serum bilirubin [mg/dL]) + 11.2*loge(INR) = 9.6*loge(serum creatinine [mg/dL]} + 6.4
- The MELD score is calculated using the international normalized ratio (INR), serum creatinine (most heavily weighted), and serum bilirubin.2
- This scoring system replaced the use of the CPT score for organ allocation in 2002.2
- The Mayo Clinic originally developed it to predict three-month mortality following transjugular portosystemic placement, but it was later expanded for use in the broader demographic.
- A higher MELD score is correlated with more severe chronic liver disease and an increased 90-day mortality: the lower limit is 6, and the upper limit is 40+.
- It helped to transition organ allocation from a system based on time accrued on the waiting list to prioritizing those with the highest expected short-term mortality.
- It was a better predictor of three-month mortality in waitlisted patients.
- It reduced waitlist time with no change in longer-term outcomes for patients or grafts.
- It transitioned to entirely objective variables, which were standardized and easily reproducible.
- It emphasized the impact of reduced renal function on survival (e.g., patients with rapidly progressing acute kidney injury due to hepatorenal syndrome type 1 have a very poor 90-day prognosis)
- Patients with worse prognoses were given higher priority for LT, as reflected by the higher median MELD scores at the time of transplant and no reduction in one-year survival of the recipient or graft.
- Problems with the MELD score included discrepancies in mortality rates between sexes and across the range of high-risk patient subpopulations (e.g., hepatopulmonary syndrome, hepatocellular carcinoma, and portopulmonary hypertension). These issues were partly corrected by the institution of “MELD exception points” in 2019.3
MELD Sodium (MELD-Na) Score Link
MELD-Na = MELD + 1.32 * (137-Na) – [0.033*MELD * (137-Na)]
- This is an updated version (2019) of the MELD score, which includes serum sodium (Na), a marker of disease severity and an independent predictor of waitlist mortality.
- Problems still include the inability to address the sex discrepancy and the fact that the serum Na fluctuates with diuretic use and intravascular volume status.
- MELD-Na was used primarily up until 2023 and was replaced by the MELD 3.0.
MELD 3.0 Score Link
MELD 3.0 = 1.33 if female + 4.56 * loge bilirubin + 0.82 * 137 − Na − 0.24 * 137 − Na * loge bilirubin + 9.09 * loge INR + 11.14 * loge creatinine + 1.85 * 3.5 ‐ albumin − 1.83 * 3.5 − albumin * loge creatinine +6
- This replaced the MELD-Na score in 2023 and includes other variables found to play a part in predicting mortality, including the role played by the current sex.
- This version updates the calculated coefficients for previous variables and recognizes that some of them interact (e.g., bilirubin and sodium and albumin and creatinine).
- It is an improved predictor of waitlist mortality.
PELD Link and PELD-Creatinine (PELD-Cr) Score
PELD = 4.80[serum bilirubin (mg/dL)] + 18.57[INR]-6.87[albumin (g/dl)] + 4.36(if less than 1 year of age) + 6.67(if growth failure)
- This is used to estimate the disease severity and three-month survival or need for ICU admission within three months of listing in patients under 12 years of age.
- It is calculated from the values of serum albumin, serum bilirubin, and INR. It considers the patient’s age at the time of listing (less than one year of age or greater than or equal to 1 year of age) and the presence or otherwise of growth failure (categorical measurements of height or weight more than two standard deviations below normal for age and gender).
- There were updates in 2023 which included serum creatinine (Cr) and improved the prediction of waitlist mortality. It also adjusted the scoring system to better align with the adult population.
Other Scoring Systems Used in Patients With Liver Failure
- Other scoring systems are used to formulate the prognosis of patients with acute and chronic liver disease and to predict which ones would benefit from early LT.
- The Clichy-Villejuif criteria were developed in France to estimate the need for urgent LT in hepatitis B-induced liver failure.4
- The Kings College Hospital criteria devised in 1989 looked for signs, symptoms, and test results that could identify patients with a poor enough prognosis to consider early LT.5 Link.
- MESO index: The MELD to sodium index is another system using the MELD score and serum Na to predict short- and long-term survival in patients with end-stage liver disease.
- iMELD: integrated MELD – an upgrade on the MELD score using age and serum Na.
- UKELD: United Kingdom MELD — the UK version is derived from and similar to the MELD score, again using serum Na as a variable.
- CLIF-SOFA: chronic liver failure – sequential organ failure assessment – looks at acute-on-chronic liver failure in patients with end-stage liver disease.
- APACHE II: Acute Physiology and Chronic Health Evaluation – a severity of disease classification system used predominantly in the emergency department and intensive care unit.
References
- Child CG, Turcotte JG. Surgery and portal hypertension. Major Probl Clin Surg. 1964;1: 1-85. PubMed
- Freeman R, Wiesner R, Harper A et al. The new liver allocation system: moving toward evidence-based transplantation policy. Liver Transpl. 2002;8(9): 851-8. PubMed
- Elwir S, Lake J. Current status of liver allocation in the United States. Gastroenterol Hepatol NY. 2016; 12(3): 166-70. PubMed
- Ichai P, Legeai C, Francoz C et al. Patients with acute liver failure listed for super urgent liver transplantation in France: reevaluation of the Clich-Villejuif criteria. Liver Transpl. 2015;21(4) 512-23. PubMed
- O’Grady J, Alexander G, Hayllar K, Williams R. Early indicators of prognosis in fulminant hepatic failure. Gastroenterology. 1989;97(2):439-45. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.