Copy link
Global Burden of Surgical Disease
Last updated: 01/06/2025
Key Points
- Disparities in access to surgical and anesthesia care represent a significant burden to health worldwide.
- Investment in essential surgical services worldwide is a cost-effective way to reduce morbidity and mortality in low- and middle-income countries (LMICs).
- Surgical and anesthesia care in LMICs is limited by various infrastructure challenges, including shortages of trained providers and access to surgical equipment.
Introduction to Global Surgical Disease
- Over 5 billion people worldwide lack access to safe anesthesia and surgical services, representing a critical global health crisis.1-3
- Until the 1990s, global health initiatives in resource-limited settings focused primarily on infectious diseases and undernutrition, with limited attention to surgical care. Recent evidence indicates that surgery is not only cost-effective but essential to address the increasing burden of noncommunicable diseases and injuries in LMICs.1
- In 2010, 16.9 million lives were lost due to untreated surgical conditions.2,3
- The lack of access to safe surgical care results in 4 times more deaths annually than HIV/AIDS, tuberculosis, and malaria combined.2,3
- Surgical diseases make up approximately 30% of the global disease burden. Despite this substantial impact, anesthesia and surgical care receive only 1% of total development assistance.3
- This disparity is especially severe in LMICs, where 93% of the population lacks access to basic surgical services, including emergency, trauma, and obstetric procedures.1,2
Global Disparities in Surgical and Anesthesia Care
- Despite comprising over a third of the world’s population, low-income countries account for only 6% of all surgeries performed globally.2,3
- Approximately 143 million additional surgeries are required each year worldwide to meet the current unmet need.2,3
- In LMICs, the failure to treat surgical conditions leads to approximately 4.7 million deaths annually, representing 10% of all deaths worldwide.1,3
- The true burden is likely higher, as certain common surgical conditions are not always separately classified in global health estimates. For example, injuries alone cause nearly 5 million deaths each year, many of which could be prevented with timely surgical interventions.1
- High perioperative mortality rates, with a substantial contribution from anesthesia-related deaths, remain a significant barrier in LMICs. The rate of anesthesia-related death has been estimated to be as much as 100 times higher in LMICs compared to high-income countries (HICs).2-3
- Low-income countries have perioperative mortality rates estimated to range from 0.2% to 6%, with substantial variation within countries and significantly higher mortality for emergent procedures.3
- It is estimated that the risk of anesthesia-related death for a woman undergoing an obstetric procedure in LMICs is 1.2 per 1000 procedures. Further data suggests that anesthesia-related maternal mortality for obstetric procedures is 300-fold higher for neuraxial and 900-fold higher for general anesthesia in LMICs than in the United States.3,4
- Essential surgical disorders are defined by the World Bank’s Disease Control Priorities report as those that are primarily or significantly treated through surgical procedures. These carry a substantial health burden and can be effectively managed with cost-efficient surgical care that is feasible to implement globally.1
- Expanding accessibility in LMICs to essential surgical procedures could prevent around 1.5 million deaths annually, or roughly 7% of all preventable deaths in LMICs.1,3
Economic Impacts and Issues
- Each year, 32.8 million people face catastrophic healthcare expenses due to surgical costs. This number increases to 81.2 million when including significant nonmedical expenses, such as transportation, lodging, and lost wages.2
- Patients in LMICs are particularly vulnerable to these expenses. Patients in the lowest quartile of global wealth are 61 times more likely to experience catastrophic healthcare costs compared to those in the highest wealth quartile.2
- Surgical morbidity and mortality have significant economic impacts, with estimates suggesting that untreated surgical conditions could reduce gross domestic product growth in LMICs by 2% by 2030.3
- Essential surgical procedures are among the most cost-effective health interventions, comparable to vaccinations and infectious disease treatments.1,3
- Investment in surgical services at first-level hospitals, which provide basic emergency services and are able to perform 28 essential surgical procedures, yields a benefit-cost ratio greater than 10:1.1,3
- Proper investment in essential anesthesia and surgical services in LMICs is projected to yield a financial return of $12.3 trillion by 2030.2,3
- Costs of essential surgical procedures range from $10 to $400 per disability-adjusted life year (DALY) averted (Figure 1).1,3
- These costs are often lower than other public health interventions, such as antiretroviral therapy for HIV/AIDS (approximately $900 per DALY averted) and oral rehydration therapy (more than $1000 per DALY averted).1
- Emergency obstetrical care is 3-times more cost-effective in averting DALYs than the measles vaccine.3
- Investing in essential surgical and anesthesia services in LMICs could avert an estimated 1.4 million deaths and 77.2 million DALYs annually.2,3
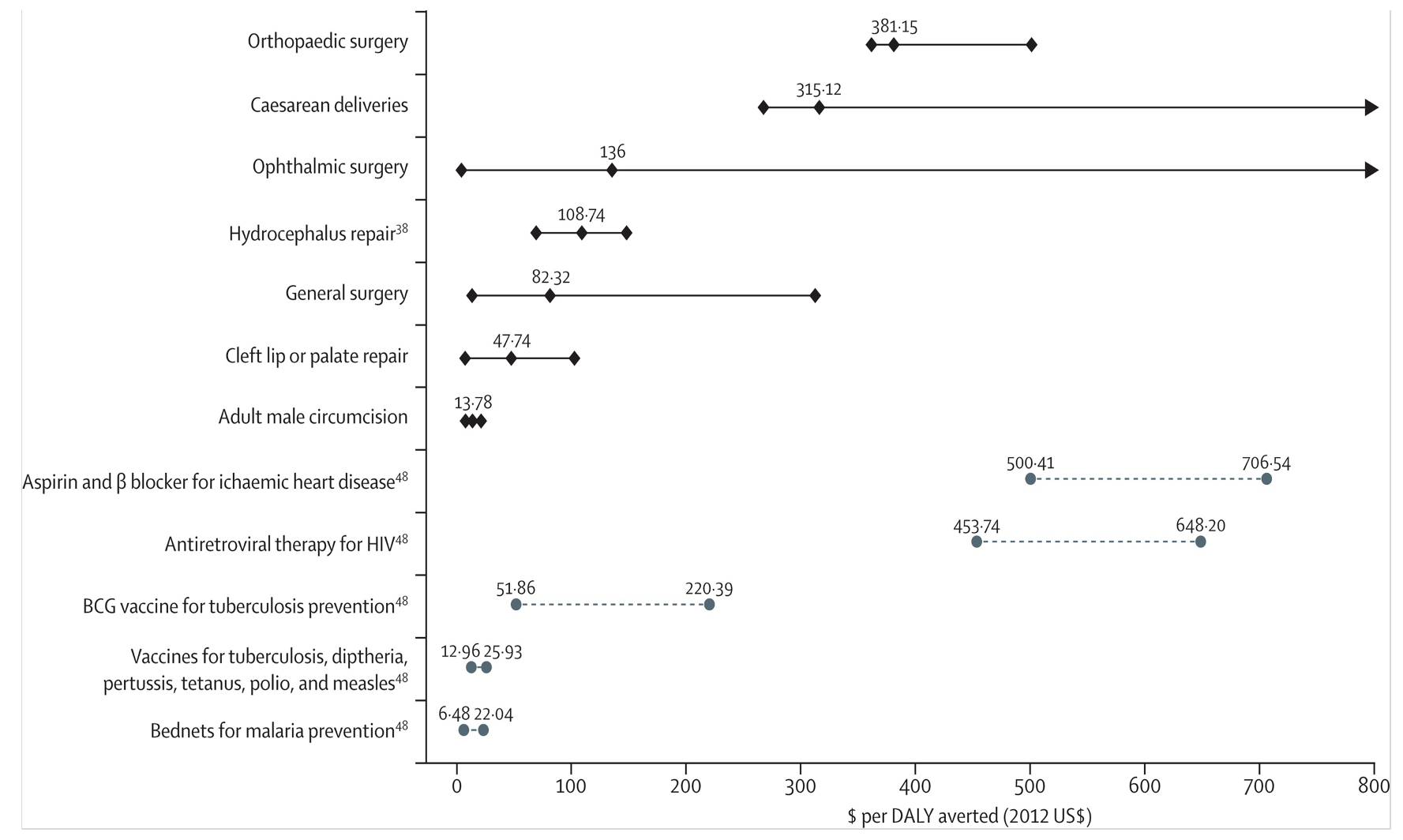
Figure 1. Cost-effectiveness of surgical intervention versus other common public health interventions. Data points are medians and error bars are ranges. The diamonds and solid lines are for surgical interventions; circles and dashed lines are other public health interventions. Source: Chao, Tiffany et al. Cost-effectiveness of surgery and its policy implications for global health: a systematic review and analysis. The Lancet Global Health, Volume 2, Issue 6, e334 - e345. CC-BY. Link
Infrastructure Challenges
- LMICs often face critical shortages of surgical personnel, with only 0.13 to 1.57 surgeons and 0.1 to 4.9 anesthesiologists per 100,000 people. In contrast, the U.S. has nine surgeons and 11.4 anesthesiologists per 100,000 people.1,2
- There is an estimated shortage of 1.1 million surgeons, 550,000 anesthesiologists, and 483,000 obstetricians globally.2
- Workforce shortages are exacerbated by resource constraints, lack of provider training capacity, and “brain drain” with migration of providers from LMICs to HICs.1-3
- A lack of essential infrastructure, including anesthesia equipment, operating rooms, and medications, is a significant barrier to safe surgical care in LMICs.1-3
- Hospitals in LMICs frequently lack functioning equipment, such as anesthesia machines, pulse oximeters, and laryngoscopes. Many hospitals have unreliable access to electricity, running water, and adequate oxygen supply.2,3
- Limited access to pain management and medications is a significant contributor to global morbidity, with 5.5 billion people lacking access to narcotic medications for analgesia.3
- Hospitals in LMICs often lack adequate space, leading to overcrowding. This and staffing shortages can lead to delays in diagnosis and initiation of medical intervention, causing nonsurgical conditions to progress to those requiring surgical intervention.2
- Poor administrative support, lack of professional management training, and weak organizational hierarchies are challenges often encountered at LMIC hospitals.2
- Additionally, corruption remains a significant concern, with 80% of people in low-income countries reporting having experienced healthcare-related corruption, such as bribes or misallocation of resources.2
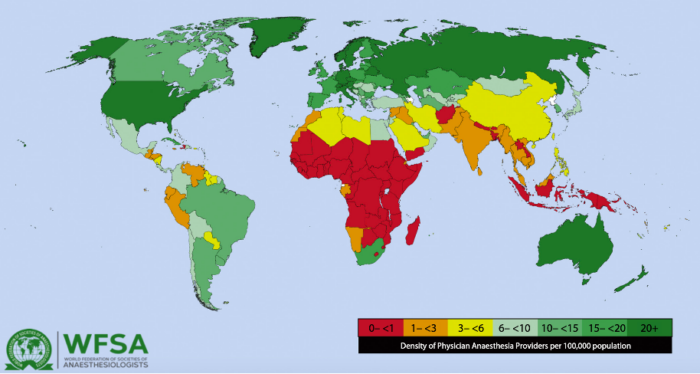
Figure 2. World Federation of Societies of Anaesthesiologists Workforce Map. Source: Kempthrone P, Morriss WW, Mellin-Olsen J, et ak. The Global Anesthesia Workforce Survey. Anesth Analg. 2017;125[3]:981-990. CC BY 4.0. Link
Policy, Advocacy, and Future Directions
- Key organizations, such as the World Health Organization (WHO), the World Federation of Societies of Anaesthesiologists, and Lifebox, work to improve global surgical outcomes through advocacy and initiatives focused on patient safety.2,3
- Areas of intervention include workforce expansion, financial risk protection for patients, and infrastructure improvements targeted at LMICs.2,3
- Achieving universal essential surgical coverage worldwide has been estimated to require an additional investment of $3 billion annually.1-3
- Despite the high cost, providing essential surgical services is considered a highly cost-effective intervention, reducing morbidity and mortality and increasing income.2,3
- Expanding training programs for anesthesia providers and incentivizing work in underserved areas are essential strategies to address workforce shortages in LMICs.1-3
- Task-sharing, where nonphysician providers are trained to deliver anesthesia care, can effectively bridge workforce gaps. However, task-sharing can also raise concerns about safety, efficacy, and role clarity, which must be carefully considered.1-3
- Locally trained nonphysician anesthesia providers have been shown to be more likely to remain in underserved areas and less likely to emigrate, which can improve access to surgical care in rural settings.1
- First-level hospitals serve as critical platforms to deliver essential surgical care and should be prioritized in national health policies given their cost effectiveness.1,3
- Emergency surgeries constitute the majority of procedures performed at first-level hospitals. Improving the quality and consistency of emergency care and basic surgical interventions is highly cost-effective in reducing morbidity and mortality.1
- High-value basic surgical procedures include laparotomies, cesarean deliveries, open fracture management, wound debridement, dilation and curettage, and closed fracture reductions.2
- Implementing safety protocols and providing basic monitoring devices has been shown to reduce perioperative mortality rates significantly.1,2
- For example, the WHO Surgical Safety Checklist, a 19-item tool designed to ensure key safety steps are followed during surgery, has been shown to reduce perioperative mortality by 47% and complications by 35%.1,2
- Improved access to anesthesia training and equipment has enhanced surgical outcomes and reduced costs in resource-limited settings.3
- The use of regional anesthesia reduces the need for advanced airway management and often decreases costs.3
- Portable anesthesia machines and oxygen concentrators can lower perioperative costs and can offer significant advantages in resource-limited settings.3
- Improvements in basic quality and safety monitoring, such as morbidity and mortality conferences, have led to better outcomes and reduced mortality in both high- and low-income countries.1
References
- Mock CN, Donkor P, Gawande A, Jamison DT, Kruk ME, Debas HT. Essential surgery: key messages from Disease Control Priorities, 3rd edition. Lancet. 2015;385(9983):2209-19. Link
- Meara JG, Leather AJ, Hagander L, et al. Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386(9993):569-624. PubMed
- Lipnick MS, Ronald MD, Geld AW. Anesthesia and Analgesia in the Global Context. In: Gropper MA et al. (eds). Miller’s Anesthesia. 9th ed. Elsevier; 2019: 10-53.
- Sobhy S, Zamora J, Dharmarajah K, Arroyo-Manzano D, et al. Anaesthesia-related maternal mortality in low-income and middle-income countries: a systematic review and meta-analysis. Lancet Glob Health. 2016 May;4(5):e320-7. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.