Copy link
Etomidate
Last updated: 05/10/2023
Key Points
- Etomidate is a carboxylated imidazole derivative used most commonly for the induction of general anesthesia. The typical induction dose is 0.2-0.6 mg/kg intravenous (IV).
- Etomidate has a short duration of action of 3-8 minutes owing to its rapid redistribution. It has no analgesic properties.
- Adverse effects include nausea/vomiting, adrenocortical suppression, pain on injection, and myoclonus.
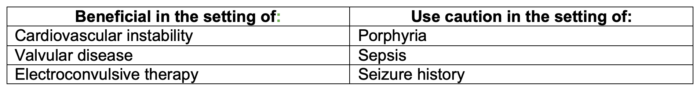
- Etomidate is most helpful in clinical scenarios where cardiac stability is required. Though systemic vascular resistance slightly decreases, cardiac output and heart rate remain stable, resulting in minimal decreases in mean arterial pressures (MAP).
Mechanism of Action and Pharmacokinetics
Mechanism of Action1
- Etomidate depresses the reticular activating system, which is responsible for wakefulness.
- It activates the gamma-aminobutyric acid (GABA) type A receptor by potentiating GABA-induced chloride currents. A second mechanism is through direct GABAA agonism.
- Specifically, etomidate potentiates GABA-mediated chloride channels via β2 and β3 on the GABA A receptor, thus causing neuronal hyperpolarization and inhibiting signaling.
Pharmacokinetics1
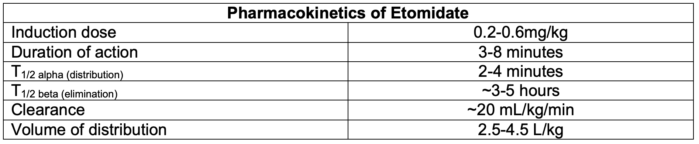
- Duration of action is dependent on redistribution of the drug from its active site.
- Metabolism is primarily accomplished in the liver by hepatic ester hydrolysis. The primary metabolite, a carboxylic acid, is inactive and water-soluble.
- Excretion is primarily through renal (85%) and biliary (13%) metabolite excretion1; less than 2-3% is excreted unchanged.
- Protein binding of etomidate is high (~75%) and mostly to albumin.
Effects on Organ Systems
Cardiovascular System2
- Cardiovascular stability with induction is the most advantageous property of etomidate.
- Cardiac output and heart rate are minimally affected. MAP is maintained or only modestly decreased due to reductions in systemic vascular resistance.
- Myocardial oxygen supply and demand stay proportional, as there is a mild decrease in coronary blood flow in addition to a decrease in myocardial oxygen requirement.1
Central Nervous System
- Etomidate is a cerebral vasoconstrictor, decreasing cerebral blood flow and cerebral metabolic rate of oxygen consumption proportionally.1
- Cerebral perfusion pressure (CPP = MAP – ICP) is preserved or increased as MAP is maintained or only minimally decreased and ICP is decreased through reduction in CBF.1
- EEG effects include initially increased α amplitude followed by progressive decrease in activity.3 These effects are thought to lengthen seizure duration, making etomidate a useful agent for electroconvulsive therapy (ECT).
- Epileptogenic foci are activated.1
Respiratory System1
- Etomidate produces less ventilatory depression compared to other IV induction agents.
- Generally, etomidate decreases tidal volumes while the respiratory rate increases.
- A short period of hyperventilation may be seen immediately postinduction followed by brief apnea.
Endocrine System1,3
- Etomidate suppresses adrenocortical production of cortisol secondary to a dose-dependent inhibition of 11-β-hydroxylase, which converts 11-deoxycortisol to cortisol and is an upstream enzyme in aldosterone production.
- Inhibition can occur after a single induction dose, and suppression lasts 4-8 hours, resulting in decreased corticosteroid levels for 24-48 hours.
Adverse Effects in Other Organ Systems1,2
- Pain on injection is a frequent side effect secondary to the propylene glycol formulation. It can be attenuated with IV lidocaine immediately prior to administration and may be accompanied by thrombophlebitis.
- Myoclonus is seen in about 30-60% of patients, possibly secondary to the imbalance of inhibitory and stimulatory signals between the thalamus and cortex. Hiccups can also occur.
- Etomidate increases the risk of postoperative nausea and vomiting.
- Porphyria attack can occur in patients with a history of porphyria.
Clinical Uses and Pearls
- Etomidate is most often used for IV induction of anesthesia. It is not commonly used for maintenance of general anesthesia or sedation in the intensive care unit (ICU) due to adrenal suppression of corticosteroid synthesis.
- Suppression of 11-β-hydroxylase induces relative adrenal insufficiency. Etomidate should be used with caution in patients with sepsis.1
- Etomidate lacks analgesic properties.
- Hemodynamic stability makes etomidate useful for patients with poor ejection fraction, coronary artery disease, or severe aortic stenosis/valvular disease.4
- Etomidate should be used with caution in patients with a history of seizures due to activation of epileptogenic foci. However, this side effect can be advantageous for ECT when increased seizure duration is desired.1
- Because etomidate causes less respiratory depression compared to propofol, it may be useful for situations where spontaneous ventilation is necessary.
References
- Jaap V, Sitsen E, Reekers M. Intravenous anesthetics. In: Gropper MA et al. Miller’s Anesthesia. 9th ed. Philadelphia: Elsevier; 2020:666-70.
- Vanlersberghe C, Camu F. Etomidate and other non-barbiturates. Handb Exp Pharmacol. 2008; 182:267-82. PubMed
- Fragen RJ, Shanks CA, Molteni A, et al. Effects of etomidate on hormonal responses to stress. Anesthesiology. 1984; 61:652-6. PubMed
- Haessler R, Madler C, Klasing S, et al. Propofol/fentanyl versus etomidate/fentanyl for the induction of anesthesia in patients with aortic insufficiency and coronary artery disease. J Cardiothoracic Vasc Anesth. 1992; 6(2):173-80. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.