Copy link
Drowning
Last updated: 11/10/2023
Key Points
- Drowning is the third leading cause of unintentional injury death worldwide and accounts for 7% of all injury-related deaths.
- Drowning causes hypoxemia, loss of consciousness, and cardiac arrest. Fluid aspiration results in lung injury and acute respiratory distress syndrome.
- Early basic life support (BLS) and advanced cardiac life support are critical.
- The duration of submersion is the most critical factor in determining outcomes.
Introduction
- Drowning is the third leading cause of unintentional injury death worldwide. It accounts for 7% of all injury-related deaths.1
- In the United States, drowning is a leading cause of death in children where swimming pools or beaches are easily accessed (California, Arizona, Florida, etc.), especially during the summer months. The highest incidence of drowning occurs in males, American Indians/Alaskan natives, children 1-4 years of age, and low socioeconomic status.2
- Risk factors for drowning are3
- male sex;
- children younger than 14 years;
- lack of supervision;
- African American or Native American;
- alcohol use;
- aquatic exposure;
- risky behavior;
- low socioeconomic status; and
- epilepsy (15-20-fold increased risk).
- In 2002, the World Congress on Drowning agreed on a consensus definition of drowning as the “process of experiencing respiratory impairment from submersion/immersion in liquid.”4
- Terms such as wet or dry drowning, near drowning, secondary drowning, active and passive drowning should be avoided.3,4
Pathophysiology
- The drowning process begins with the victim’s airway lying below the surface of the liquid (submersion) or the liquid splashes over the face (immersion), at which time the victim voluntarily holds their breath.3
- This may be followed by an involuntary period of laryngospasm secondary to the presence of liquid in the oropharynx or larynx.
- Absence of gas exchange results in hypoxia, hypercarbia, and acidemia.
- Cardiac arrest occurs from hypoxemia and is preceded by tachycardia, followed by bradycardia, pulseless electrical activity, and asystole.3
- As laryngeal spasm and obstruction abate, the victim actively aspirates the liquid.
- Fluid aspiration results in varying degrees of lung injury. The composition of the aspirated liquid is less important than the quantity. Aspiration of 1-3 mL/kg of liquid causes respiratory compromise and hypoxemia.
- Both salt water and fresh water wash out the surfactant and disrupt the alveolar capillary membrane, resulting in noncardiogenic pulmonary edema and acute respiratory distress syndrome.
- About 20% of nonfatal drowning victims suffer neurologic damage from hypoxic-ischemic injury.
- Hypothermia in cold water drowning can be protective, allowing drowning victims to survive prolonged submersion episodes.3
Treatment
Prehospital Care
- The victim should be removed from water and placed in a supine position.
- BLS should be initiated immediately.
- Since the cardiac arrest is primarily from hypoxemia, cardiopulmonary resuscitation should follow the traditional airway-breathing-circulation (ABC) sequence rather than the circulation-airway-breathing (CAB) sequence.3
- BLS includes five initial rescue breaths followed by 30 chest compressions and continuing with two rescuer breaths and 30 compressions until there are signs of life or advanced life support becomes available.3
- Cervical spine precautions should be used only when head or neck injury is suspected.
- After initial stabilization, the patient’s wet clothing should be removed and the patient should be wrapped in blankets.
- Because of the wide range of clinical presentations of drowning, a classification system of six grades (1-6) can help risk-stratify and guide interventions.3 Higher numbers indicate more severe impairment (Figure 1).
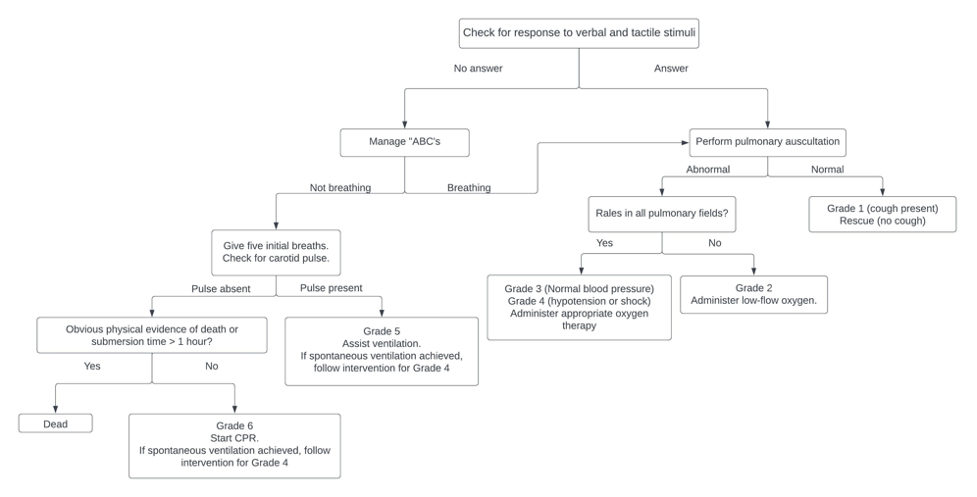
Figure 1. Initial evaluation and management of drowning victims. Adapted from Szpilman D, et al. Drowning. N Engl J Med. 2013; 3366(22): 2102-10. PubMed
In-Hospital Care (Emergency Department or Intensive Care Unit)
- Most critical role in management is the prompt correction of hypoxemia and acidosis.
- There should be a low threshold for intubation for severe hypoxia, altered mental status, or significant respiratory distress.
- Positive pressure ventilation improves hypoxemia in drowning victims. Lung protective ventilation strategies, such as low tidal volumes and positive end-expiratory pressure, should be used similar to other types of acute lung injury. Permissive hypercapnia should be avoided in patients with hypoxic-ischemic brain injury.
- There is no role for routine bronchoscopy or glucocorticoid therapy in drowning victims.
- Vomiting is common in victims given swallowing large amounts of water and positive pressure ventilation during resuscitation. An orogastric or nasogastric tube should be inserted for gastric decompression.
- In patients who recover quickly, mechanical ventilation should be continued for at least 24 hours, even when pulmonary gas exchange appears to be adequate.3
- In patients with persistent hypoxemia despite optimal ventilator management and who did not suffer a prolonged cardiac arrest, venovenous extracorporeal membrane oxygenation can be considered on a case-by-case basis, if available.
Predictors of improved outcome include:5
- Immersion time less than 6 minutes (most critical factor)
- Younger age
- In-water resuscitation (by trained lifesaving personnel)
- Early basic and advanced cardiac life support
Water temperature and salinity have no correlation with the overall outcome.
References
- World Health Organization. Drowning. 2021. Accessed October 2023. Link
- Karaye IM, Farhadi K, Sengstock G, et al. Recent trends in fatal unintentional drowning rates in the United States, 1999-2020. J Safety Res. 2023; 84:411. PubMed
- Szpilman D, Bierens JJLM, Handley AJ, et al. Drowning. N Engl J Med. 2013; 3366(22): 2102-10. PubMed
- Van Beeck E, Branche C, Szpilman D, et al. A new definition of drowning: towards documentation and prevention of a global public health problem The global burden of drowning. Bull World Health Organ. 2005;83(11). PubMed
- Quan L, Mack CD, Schiff MA. Association of water temperature and submersion duration and drowning outcome. Resuscitation. 2014;85(6):790-4. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.