Copy link
Coronary Artery Calcifications
Last updated: 06/21/2024
Key Points
- Coronary artery calcification (CAC) is an indicator of atherosclerosis.
- The severity of coronary artery calcification correlates with adverse postoperative outcomes.
- The coronary artery calcium score, along with other risk prediction scores, can help identify high-risk patients for targeted optimization.
Epidemiology of Coronary Artery Calcification
- CAC is a hallmark of advanced atherosclerosis and arises concomitantly with the progression of an atherosclerotic plaque (Figure 1).
- The intimal layer of coronary endothelium becomes calcified by chondrocyte-like cells secondary to an inflammatory cascade initiated by cytokines and macrophages.1
- The extent of CAC correlates closely with the degree of atherosclerosis and the likelihood of future major adverse cardiac events (MACE).1,2
- Greater than 90% of men and 67% of women aged over 70 years have CAC.8
- Risk factors associated with the development of CAC include obesity, hypertension, abnormal lipid profiles, diabetes mellitus, a familial history of CAC, chronic kidney disease, elevated fibrinogen levels, and increased C-reactive protein levels.8,9
Coronary Artery Calcification and Coronary Artery Disease
- CAC is highly prevalent in patients with coronary artery disease (CAD) and, when present, correlates with adverse post-surgical outcomes.3-7
- CAC detection via chest computed tomography (CT) scan directly identifies CAD (Figure 2) and better predicts future major adverse cardiac events in asymptomatic patients than traditional risk factors and biomarkers.1,2
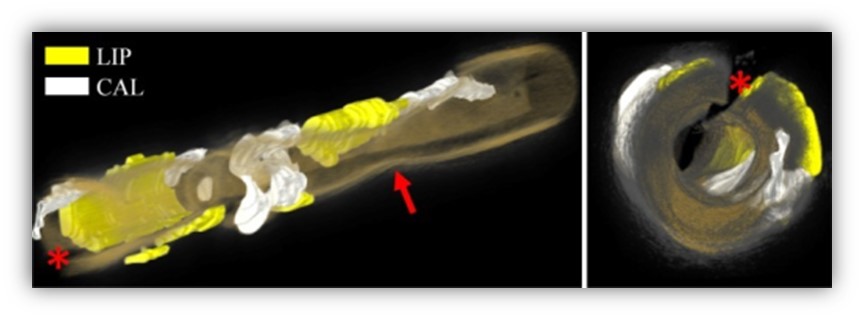
Figure 1. 3D rendering of an artery depicting lipid and calcium plaque components. The red arrow points to a stenosis. The red asterisk indicates a guide-wire shadowing artifact. Color coding: yellow = lipid-rich, white = calcific tissue, and orange-to-gray rendering of the vessel wall. Source: Ughi GJ, et al. Biomed Opt Express. 2013. Open Access. Link
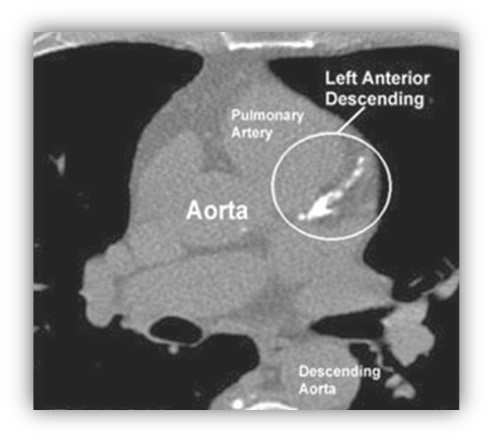
Figure 2. Extensive coronary artery calcifications warranting aggressive medical management for atherosclerosis. Source: Budoff MJ, et al. Vasc Health Risk Manag. 2008;4(2):315-24. Originally published by and used with permission from Dove Medical Press Ltd. Link
Coronary Artery Calcium Scoring
- Several large cohort studies have established that CAC independently predicts long-term cardiovascular events.1,2
- CAC is measured and scored using ECG-gated non-contrast chest CT; the scan is coupled or gated to the cardiac cycle via an ECG to diminish motion artifact. This imaging technique enables the calculation of the Coronary Artery Calcium Score (CACS) or Agatston score, offering a quick and straightforward assessment method (Table 1).
- The cumulative CACS is obtained by summing the scores of all calcified lesions, which are adjusted for sex and race and expressed as a percentile. CACS is computed separately for each coronary artery.9
- These non-contrast CT scans have few contraindications, require no patient preparation, and use small doses of radiation. The CACS aligns directly with the extent of coronary atherosclerosis, making it a valuable indicator of future MACE.1,2,9
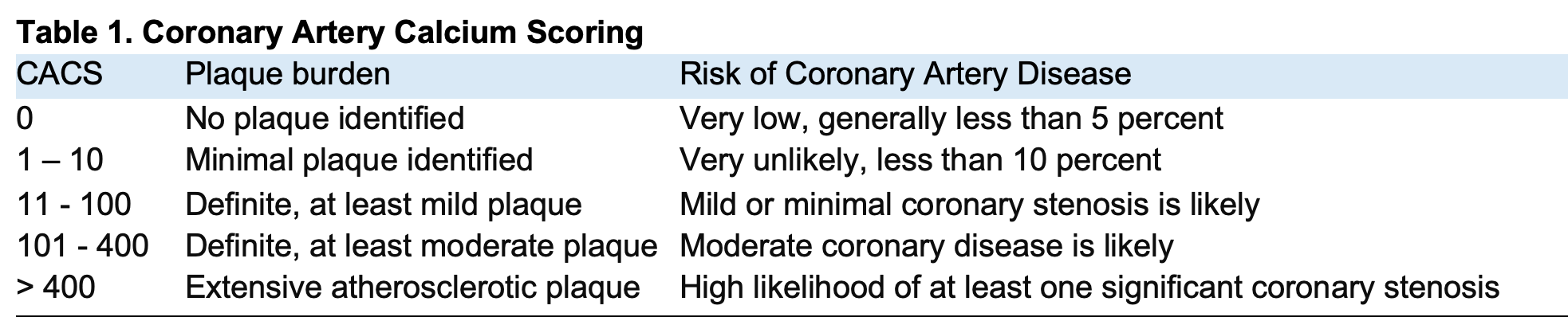
CACS = Coronary Artery Calcium Score
Hemodynamic Implications of Coronary Artery Calcium and Medical Management
- Autoregulation in the coronary arteries helps maintain a relatively constant flow to the myocardium over various pressures (~60–120 mmHg).11
- CAC compromises vasomotor autoregulatory responses. Furthermore, diminished vascular compliance in calcified arteries hampers their ability to adapt blood flow to changes in blood pressure.10,11
- Patients with heavily calcified coronaries are at an increased risk of experiencing myocardial ischemia, even with a mild drop in diastolic blood pressure.10
- While CAC indicates the presence of atherosclerosis, vascular remodeling often maintains lumen patency.9 Rarely, calcified nodules protrude into the arterial lumen, disrupting the endothelium and underlying collagen matrix, leading to coronary thrombosis.
- The mechanism by which calcified nodules contribute to acute coronary syndrome accounts for only a minority (2 – 7%) of cases. Therefore, CAC should primarily be considered a marker of atherosclerosis rather than an indicator of stenosis severity.8
- CACS surpasses traditional risk markers and helps guide treatment. Known as “ABCDE,” this framework is intended for primary prevention in high-risk patients (e.g., CACS > 100) and includes aspirin, maintaining systolic blood pressure below 120 mmHg, achieving LDL-Cholesterol levels below 55 mg/dl, Diabetes control, and optimizing Diet and Exercise.2
Coronary Artery Calcium and Postoperative Cardiac Complications
- Patients with significant CACS have a higher risk of postoperative cardiac complications, including myocardial infarction.4,5
- Routine cardiac evaluation, such as ECG, echocardiography, and thallium SPECT, may not help predict postoperative cardiovascular issues.5
- The Existing Non-gated CT Coronary Calcium Predicts Operative Risk in Patients Undergoing Noncardiac Surgeries (ENCORES) study investigated patients undergoing major noncardiac surgery.3
- Over 60% of patients had identifiable CAC, including 30% with moderate or severe CAC.
- The left anterior descending artery was most affected.
- Perioperative major clinical events after noncardiac surgery, defined as all-cause death or myocardial infarction within 30 days of surgery, occurred in 5.2% of patients.
- A higher CAC burden correlated with perioperative major clinical event rates.
Preoperative Risk Assessment and Coronary Artery Calcium Detection
- Preoperative evaluation is a crucial step in identifying and lowering the risks of cardiovascular complications in surgical patients. This assessment should include a review of the patient’s previous chest CT scans. ECG-gated and standard non-contrast chest CT scans are reliable for detecting CAC, especially in asymptomatic individuals.1,2,8,9
- Detecting CAC can help prompt aggressive risk factor modification and treatment to prevent the complications of CAD.5,7 Several studies have demonstrated the predictive value of preoperative CAC assessment in different surgical populations.4-7 Moreover, integrating existing non-gated chest CT imaging for coronary calcium assessment with the revised cardiac risk index is a promising tool for enhancing preoperative risk stratification.3
- Identifying CAC preoperatively, regardless of symptomatology, is imperative to reduce perioperative cardiac risks. Incorporating CAC assessment into preoperative protocols can help identify high-risk patients and implement targeted management strategies. These strategies include both aggressive medical treatment and invasive revascularization techniques, leading to improved cardiac risk profiles.5,7
References
- Onnis C, Virmani R, Kawai K, et al. Coronary artery calcification: Current concepts and clinical implications. Circulation. 2024;149(3):251-66. PubMed
- Selvam PV, Grandhi GR, Leucker TM, et al. Recent advances in cardiovascular risk assessment: The added value of non-invasive anatomic imaging. J Cardiovasc Comput Tomogr. 2024;18(2):113-9. PubMed
- Choi DY, Hayes D, Maidman SD, et al. Existing non gated CT coronary calcium predicts operative risk in patients undergoing noncardiac surgeries (ENCORES). Circulation. 2023;148(15):1154-64. PubMed
- Mahla E, Vicenzi MN, Schröttner B, et al. Coronary artery plaque burden and perioperative cardiac risk. Anesthesiology. 2001;95(5):1133-40. PubMed
- Kong YG, Kang JW, Kim YK, et al. Preoperative coronary calcium score is predictive of early postoperative cardiovascular complications in liver transplant recipients. Br J Anaesth. 2015;114(3):437-43. PubMed
- Grobben RB, van Waes JAR, Leiner T, et al; CHASE Investigators. Unexpected cardiac computed tomography findings in patients with postoperative myocardial injury. Anesth Analg. 2018;126(5):1462-8. PubMed
- Machino R, Shimoyama K, Oku K, et al. Prevalence of coronary calcification on preoperative computed tomography and its management in thoracic surgery. Surg Today. 2023;53(1):62-72. PubMed
- Al-Shaibi K, Bharadwaj A, Mathur A, et al. Management of calcified coronary lesions. US Cardiology Review. 2024;18:e01. Link
- Cheong BYC, Wilson JM, Spann SJ, et al. Coronary artery calcium scoring: an evidence-based guide for primary care physicians. J Intern Med. 2021;289(3):309-24. PubMed
- Parab SY, Patil VP, Shetmahajan M, et al. Coronary artery calcification on chest computed tomography scan - Anaesthetic implications. Indian J Anaesth. 2019;63(8):663-666. PubMed
- Goodwill AG, Dick GM, Kiel AM, et al. Regulation of coronary blood flow. Compr Physiol. 201716;7(2):321-382. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.