Copy link
Cardiac Tumors
Last updated: 08/19/2024
Key Points
- Pediatric cardiac tumors are rare and typically benign.
- Rhabdomyomas are the most common lesion in children, whereas atrial myxomas are the most common in adults.
- Medical versus surgical management depends on the tumor type and the patient’s presentation. When surgical intervention is indicated, anesthetic management is tailored to the patient’s lesion and symptomatology.
Introduction
- Pediatric cardiac tumors are rare, and the incidence is difficult to define.1
- Tumors can arise from any tissue in the heart and can be found in any chamber. They may be primary or secondary from local spread or metastasis.
- Most cardiac tumors in pediatrics are benign.1
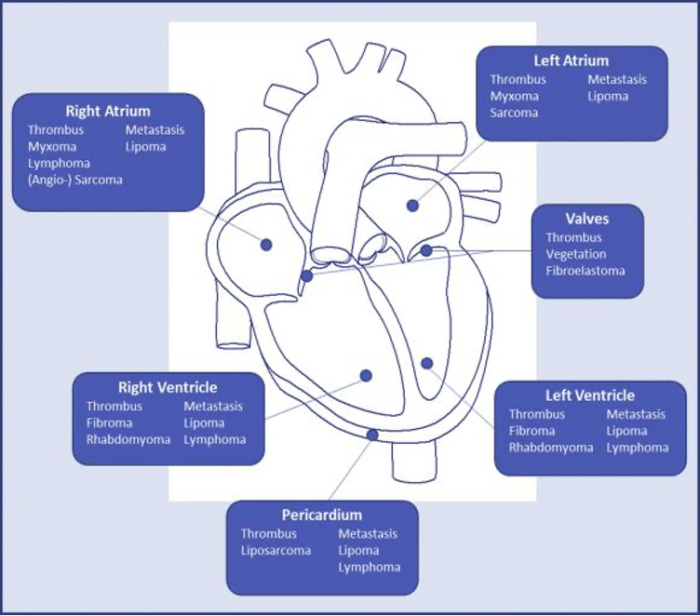
Figure 1. Cardiac Tumors: common types and locations.2 Source: Cardiac Tumors licensed under CC BY-NC-ND 4.0.
Pathophysiology
Rhabdomyoma1,2
- Rhabdomyomas are the most common cardiac tumors in children. They can occur in any heart chamber and are most commonly associated with tuberous sclerosis.
- Tumors are typically multiple and appear in utero with regression after birth; thus, serial echocardiograms are recommended.
- Clinical presentation can include palpitations or syncope due to arrhythmogenic nature or heart failure when obstruction is present.
- Surgical intervention may be necessary for patients with intractable arrhythmias or heart failure; asymptomatic patients are monitored for regression of tumors.
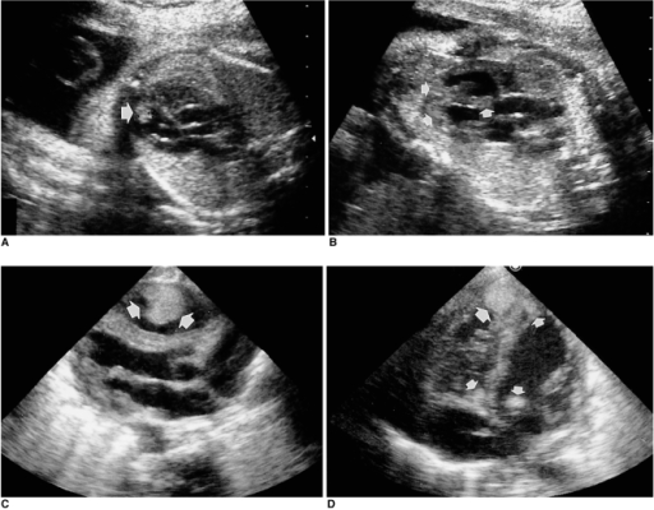
Figure 2. Prenatal (A&B) and postnatal (C&D) echocardiographic images of an infant with multiple rhabdomyomas. Arrows indicate masses. Figures reproduced from Prenatal ultrasound findings of fetal neoplasms licensed under CC BY-NC 3.0.
Fibroma1,2
- Fibromas are the second most common cardiac tumor in children. They are slow-growing tumors located most commonly in the ventricular myocardium.
- Arrhythmias or sudden cardiac death are possible due to conduction abnormalities.
- Surgical resection is recommended because fibromas do not spontaneously regress. Palliation with partial resection may be performed if complete removal would lead to impaired cardiac function.

Figure 3. Transthoracic echocardiogram showing an intraventricular septal mass (M). RA: right atrium, RV: right ventricle, LV: left ventricle. Figure reproduced from Successful surgical treatment for recurrent cardiac fibroma 21 years after resection licensed under CC BY 4.0.
Myxoma1,2
- Myxomas are the most common cardiac tumor in adults but rarely occur in children. They are most commonly located in the left atrium, with 70% of cases in females and the mean age at diagnosis of 50 years.
- An echocardiogram typically shows a mobile mass attached to the endocardium with a stalk.
- Resection is performed to prevent potential complications such as mitral valve obstruction or embolic events.
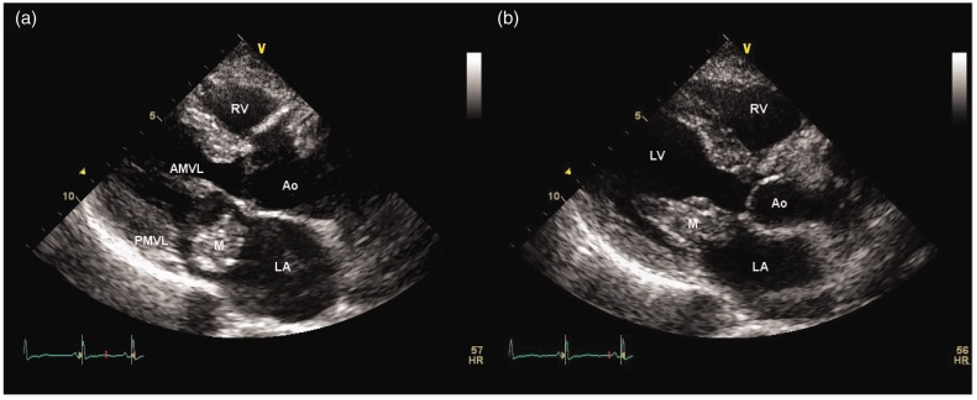
Figure 4. Transthoracic echocardiogram of a left atrial myxoma (M) seen in the left atrium (a) and prolapsing the mitral valve (b). LA: left atrium, LV: left ventricle, RV: right ventricle, Ao: aorta, AMVL: anterior mitral valve leaflet, PMVL: posterior mitral valve leaflet Reproduced from Atrial myxoma masquerading as Takayasu’s arteritis licensed under CC BY-NC 3.0.
Teratoma1
- Teratomas are uncommon midline tumors that most commonly occur in the sacral region, followed by the mediastinum. They are nonmalignant in nature but require surgical resection for treatment.
- These tumors usually arise in the anterior mediastinum, but the involvement of the heart and great vessels can occur with large tumors.
Cardiac Hemangioma1
- Hemangiomas can occur anywhere in the heart.
- They may be asymptomatic and may regress or respond to medical treatment. Patients should be referred to a vascular malformation clinic for management.
- Surgical intervention may be necessary depending on location and symptoms.
Primary Malignant Cardiac Tumor3
- Malignant cardiac tumors are extremely rare in pediatrics.
- Sarcoma is the most common primary malignant tumor, followed by malignant germ cell tumors and lymphoma.
- Sarcomas are managed with surgical excision, whereas lymphoma is treated with chemotherapy.
- Recurrence of cardiac sarcoma after resection is common and carries a poor prognosis.
Secondary Cardiac Tumor
- Metastasis to the heart is possible with nearly any type of malignancy and can occur late in a patient’s course. Depending on the type of malignancy, spread can occur in many different ways: via blood, lymphatics, transvenous, or direct invasion.
- Treatment options depend on the type of secondary tumor and include a combination of chemotherapy, radiation, and surgical resection or palliation.4
- Wilms’ tumor is the most common pediatric tumor with vascular extension to the heart; other tumors such as renal clear cell, adrenal tumors, and hepatoblastoma can present similarly. If the tumor extends into the right atrium, cardiopulmonary bypass (CPB) is frequently required during surgical resection.5
Diagnosis
Clinical Presentation
- Presentation is variable. Approximately 7% of cases are asymptomatic.
- The most common symptoms include dyspnea, chest pain, and cyanosis.
- Findings on an exam are typically murmurs, congestive heart failure, and arrhythmias.3
Diagnostic Studies
- Echocardiography is the mainstay of diagnosis to evaluate the lesion and determine its impact on circulation.
- Magnetic resonance imaging (MRI) can be used to provide a more detailed delineation of tissues.1,2
- Patients with significant arrhythmias may undergo electrophysiology studies +/- ablation.
Treatment Strategies
Medical Management1
- Rhabdomyomas tend to regress spontaneously and can be followed with serial echocardiography.
- Hemangiomas may regress and may be managed medically. These patients are referred to a vascular malformation clinic for management.
Surgical Management
- Surgical resection of fibromas is indicated due to the potential for sudden cardiac arrest.2
Anesthetic Considerations for Interventional/Surgical Management
Preoperative
Labs
- Complete blood cell count
- Basal metabolic profile to assess renal function and electrolyte disturbances if on diuretics
- Type and crossmatch for surgical procedures
Diagnostics
- ECG, echocardiography +/- MRI
- Chest radiograph
Intraoperative
Monitoring
- Standard American Society of Anesthesiologists monitors, plus additional monitors utilized for CPB cases
- Transesophageal echocardiogram
Access
- Peripheral and central venous access: Consideration of the tumor location will determine appropriate locations for intravenous access placement. For example, lesions involving the inferior vena cava, such as Wilms’ tumor, require upper extremity venous access.1
- Arterial line
- Central venous line
Anesthesia Technique
- No specific general anesthetic technique is required for cardiac tumors.
- The anesthetic is tailored to the patient’s hemodynamics.
Hemodynamic Goals (Induction, Pre-CPB, Post-CPB)
- Dependent on specific lesion’s hemodynamic effects
- Maintenance of age-appropriate vital signs
- Special CPB considerations: none
Postoperative
- Standard postcardiac surgery intensive care monitoring
- Potential complications include arrhythmias, heart failure, low cardiac output syndrome, etc.3
References
- Andropoulos DB, Stayer SA, Mossad EB, et al. Anesthesia for Miscellaneous Cardiac Lesions. In: Anesthesia for Congenital Heart Disease, 3rd Edition. Hoboken, NJ: John Wiley & Sons; 2015:622-5.
- Tyebally S, Chen D, Bhattacharyya S, et al. Cardiac tumors: JACC CardioOncology State-of-the-Art Review. JACC CardioOncol. 2020;2(2):293-311. PubMed
- Tzani A, Doulamis IP, Mylonas KS, Avgerinos DV, Nasioudis D. Cardiac tumors in pediatric patients: A systematic review. World J Pediatr Congenit Heart Surg. 2017;8(5):624-32. PubMed
- Yanagawa B, Chan EY, Cusimano RJ, Reardon MJ. Approach to surgery for cardiac tumors: Primary simple, primary complex, and secondary. Cardiol Clin. 2019;37(4):525-31. PubMed
- Fanelli MCA, Guilhen JCS, Duarte AAB, et al. Management of pediatric tumors with vascular extension. Front Pediatr. 2022;9:753232. PubMed
Other References
- Christensen J. Congenital Cardiac Anesthesia Society. Intracardiac Masses. Accessed August 2, 2024. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.