Copy link
Burnout and Wellness
Last updated: 02/06/2025
Key Point
- Burnout remains a prevalent occupational hazard among anesthesiology professionals, significantly impacting their careers and well-being.
- Healthcare system stressors, patient safety incidents, and psychological strain create a self-perpetuating burnout cycle that degrades performance, quality, and worker well-being.
- Wellness programs with integrated peer support programs provide essential services that combat burnout and restore healthcare workers' well-being, enabling compassionate patient care.
- Establishing peer support programs that provide “emotional first aid” for patient safety events creates both immediate interventions and lasting cultural changes toward compassionate healthcare delivery.
Introduction
- Burnout is a significant occupational hazard among anesthesiology professionals, characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment. Studies indicate that approximately 40-67% of anesthesiology professionals experience burnout symptoms at some point in their careers.1,2
- Definition of burnout (Maslach Burnout Inventory)3
- Emotional exhaustion: Feeling emotionally drained and depleted
- Depersonalization: Detachment from patients and colleagues
- Reduced personal accomplishment: Decreased sense of competence and achievement
- Key Statistics
- Burnout rates among healthcare professionals: 46%4
- High-risk rates for burnout among anesthesiology professionals: 40-67%1,2
- Median rate of burnout of anesthesiology residents: 24%5
- The Reinforcing Loop: Burnout is exacerbated by a reinforcing loop of three major factors. This is destructive and nonsustainable in the cultural setting of professional stoicism, blame, and shame and in the absence of a structured institutional support response (Figure 1).
- System stressors: Chronic exposure to and participation in dysfunctional and suboptimized care systems and processes
- Unintended adverse medical events, medical error, and patient injury: Exposure to patient harm often resulting from system and process failures
- Second victim phenomenon: Second victims are individuals working within an environment to offer/provide care and are traumatized by exposure to clinically challenging cases and events.6
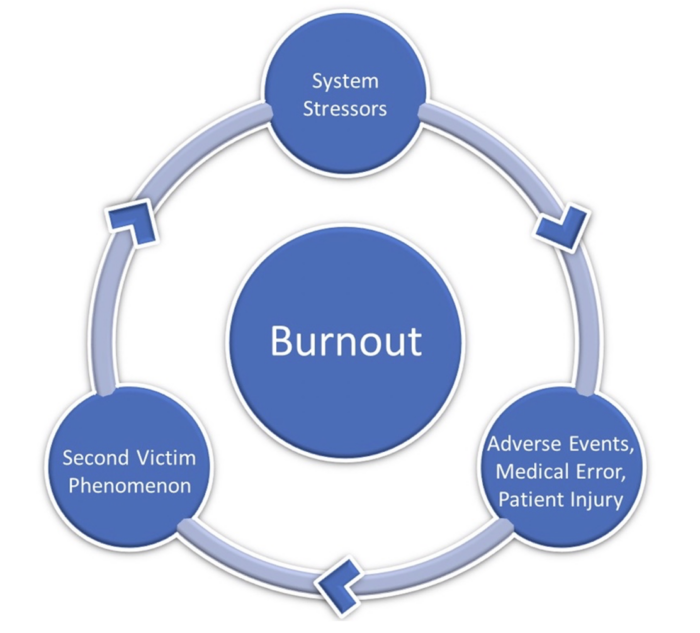
Figure 1. The reinforcing loop of burnout
Risk Factors
- System stressors
- Fragmented and suboptimized care processes
- Long work hours (more than 60 hours/week)
- High-stress environment and critical decision-making
- Night/weekend call responsibilities
- Work-life imbalance
- Production pressure and case volumes
- Medico-legal concerns
- Adverse medical events, medical errors, and patient injury
- Estimated incidence of patient deaths due to medical error in the US: more than 250,000/yr7
- One in five Americans have personally experienced a medical error while receiving healthcare.8
- Examples
- Unexpected or untimely patient death
- Medication error
- Wrong-site surgery
- Second victim phenomenon (Table 1)
- Among anesthesiology professionals, the prevalence of second victims ranges from 60 to 84%.9,10
- High-risk clinical situations: High-pressure, dynamic practice settings and the likelihood of involvement in adverse events due to the nature of the specialty
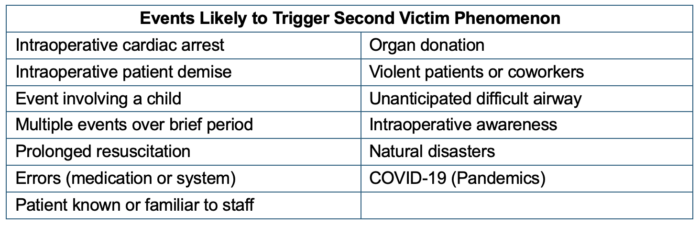
Table 1. Events likely to trigger the second victim phenomenon.12
Impact
- Healthcare professionals
- Second victims may experience symptoms in both physical and psychosocial domains (Table 2).
- The duration of symptoms varies; for anesthesia professionals, it has been demonstrated that 18% of anesthesiologists and 12% of certified registered nurse anesthetists (CRNAs) experienced symptoms for one month after the event. Additionally, 19% of anesthesiologists and 17% of CRNAs reported never fully recovering.11,13
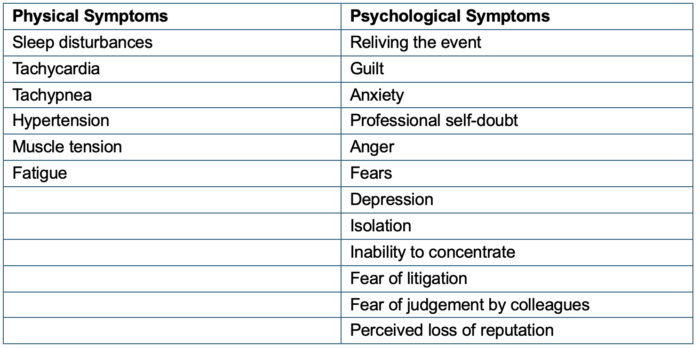
Table 2. Possible second victim physical and psychosocial symptoms10
- Second victims may also experience compromised ability to provide safe care after an event: 67% of anesthesiologists and 64% of CRNAs reported this for up to 4 hours after the event.9,11
- Quality, safety, and performance
- Compromised patient safety
- Increased medical errors
- Reduced patient satisfaction
- Loss of joy in work
- Decreased productivity
- Higher turnover rates
- Increased healthcare costs
Prevention and Management: Creating a Wellness Program with Peer Support
- Peer support: “Emotional first aid” for hospital staff involved in patient-related adverse events and stressful situations
- Peer support principles
- Acknowledge and support emotional distress
- Leverage collegial credibility
- Attentive listening
- Compassion
- Preferred source of emotional support for healthcare providers after an adverse event (Figure 2)
- Peer support principles
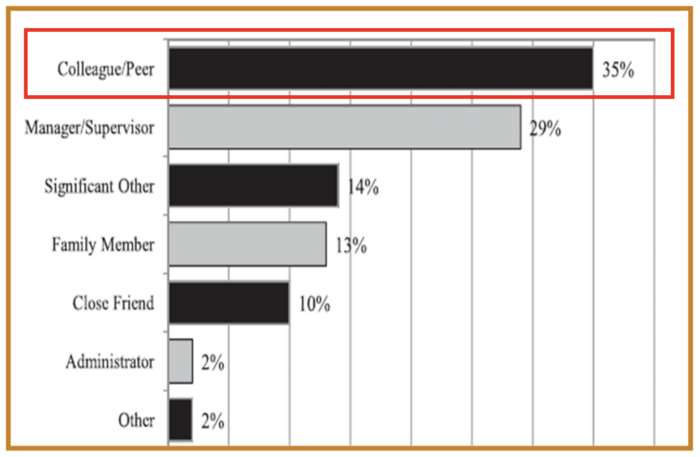
Figure 2. Preferred source of emotional support after an adverse event. Used with permission from Scott SD et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf 2010;36(5):233-240.12
-
- When implementing second victim peer support programs, specific steps should be followed to facilitate success (Table 3).
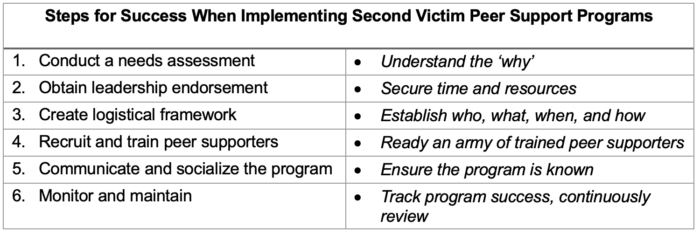
Table 3. Steps for implementing peer support programs. Adapted with permission from Finney RE, Jacob AK. Peer support and second-victim programs for anesthesia professionals involved in stressful or traumatic clinical events. Adv Anesth 2023;41(1):39-5213
- Peer support programs for adverse medical events and the second victim
- Structured peer support program
- Confidential counseling services
- Crisis intervention teams
- Peer support principles integrated into care improvement initiatives
- Understand the importance of qualitative data
- Create conditions for psychological safety
- Mitigate the role of conflict in problem-solving
- Establish equitable connections
- Build relationships and trust
- Elicit critical system sources of stressors
- Create conditions that support wellness
- Organizational level
- Leadership engagement
- Promoting work-life balance
- Recognition programs
- Wellness committees
- Peer support programs
Professional Recommendations
- Implement comprehensive wellness programs
- Reduce administrative burden
- Promote organizational culture change
- Strengthen the peer support network
References
- Afonso AM, Cadwell JB, Staffa SJ, et al. U.S. attending anesthesiologist burnout in the postpandemic era. Anesthesiology 2024;140(1):38-51. PubMed
- Lea J, Doherty I, Reede L, et al. Predictors of burnout, job satisfaction, and turnover among CRNAs during COVID-19 surging. AANA J 2022;90(2):141-147. PubMed
- Maslach C, Jackson SE, Leiter MP. Maslach Burnout Inventory Manual. 3rd ed. Consulting Psychologists Press; 1996.
- Chong MYF, Lin SHX, Lim WY, et al. Burnout in anaesthesiology residents: a systematic review of its prevalence and stressors. Eur J Anaesthesiol 2022;39(4):368-377. PubMed
- Nigam JA, Barker RM, Cunningham TR, et al. Vital signs: health worker–perceived working conditions and symptoms of poor mental health — Quality of Worklife Survey, United States, 2018–2022. MMWR Morb Mortal Wkly Rep 2023;72:1197-1205. PubMed
- Scott SD. Shifting culture through structured organizational second victim support. In: Davidson J, ed. Workplace Wellness: A Primer for Leaders in Healthcare: Supporting Clinicians from Resiliency to Suicide Prevention. Springer Publishing; 2023.
- Makary MA, Daniel M. Medical error—the third leading cause of death in the US. BMJ 2016;353:i2139. PubMed
- NORC at the University of Chicago and IHI/NPSF Lucian Leape Institute. Americans' Experiences with Medical Errors and Views on Patient Safety. Institute for Healthcare Improvement and NORC at the University of Chicago; 2017.
- van Pelt M, Smeltzer SC, van Pelt F, et al. Preliminary psychometric evaluation of the Nurse Anesthesia and the Aftermath of Perioperative Catastrophes Survey and the Ways of Coping Questionnaire. AANA J 2019;87:441-449. PubMed
- Finney RE, Jacob AK, Johnson J, et al. Implementation of a second victim peer support program in a large anesthesia department. AANA J 2021;89(3):235-244 PubMed
- Gazoni FM, Amato PE, Malik ZM, et al. The impact of perioperative catastrophes on anesthesiologists: results of a national survey. Anesth Analg 2012;114:596-603. PubMed
- Scott SD, Hirschinger LE, Cox KR, et al. Caring for our own: deploying a systemwide second victim rapid response team. Jt Comm J Qual Patient Saf 2010;36(5):233-240. PubMed
- Finney RE, Jacob AK. Peer support and second-victim programs for anesthesia professionals involved in stressful or traumatic clinical events. Adv Anesth 2023;41(1):39-52. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.