Copy link
Blood Pressure Physiology and Control
Last updated: 01/03/2025
Key Points
- Blood pressure control is a complex phenomenon. Short-term regulation is mediated via neural reflexes involving chemoreceptors and baroreceptors that can rapidly adjust heart rate, vascular resistance, and cardiac output.
- Intermediate blood pressure control is mediated via the renin-angiotensin-aldosterone system in response to fluid status, electrolyte levels, and renal perfusion.
- Long-term regulation involves hormonal and renal mechanisms.
- Anesthesia can influence these regulatory systems and attenuate the autonomic neural responses. Anesthetic agents can cause a decrease in systemic vascular resistance, reduced cardiac contractility, and hypotension.
Systolic, Diastolic, Mean, and Perfusion Pressure
Systolic Blood Pressure (SBP)
- SBP is the measure of pressure on the arterial walls upon contraction of the heart to pump blood throughout the body.1
- SBP is the pressure heard at the first Korotkoff sound during blood pressure measurement, with normal SBP being less than 120 mmHg and elevated as 130 mmHg or higher.1
Diastolic Blood Pressure (DBP)
- DBP is the measure of pressure on the arterial walls upon relaxation of the heart in between contractions at the time of closure of the aortic valve.1
- Adequate DBP is essential for coronary perfusion from coronary arteries being open, allowing coronary blood flow through the relaxed heart.1
- Normal DBP ranges between 60 and 90 mmHg, with values greater than 90 reflecting diastolic hypertension.3 Values less than 60 are associated with increased cardiovascular disease risk due to less coronary perfusion (higher in patients with pre-existing coronary artery disease).2
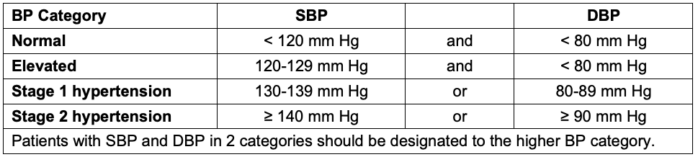
Table 1. Abbreviations: BP, blood pressure; SBP, systolic blood pressure; DBP, diastolic blood pressure. Categories of BP in adults. Adapted from Whelton PK et al. Hypertension. 2018;71(6):1269-1324. PubMed
Mean Arterial Pressure (MAP)
- MAP is the average pressure in a patient’s arteries during one cardiac cycle and is used as a measure of perfusion to vital organs.1

Perfusion Pressure
- Perfusion pressure is the pressure gradient that is the driving force to organs and tissues.4 There are different examples of perfusion pressures
- Mean arterial pressure (MAP): described above
- Ocular perfusion pressure (OPP): Pressure driving blood flow to the eye4
- OPP = MAP – IOP (intraocular pressure)4
- Coronary perfusion pressure (CoPP): Blood flow to the myocardium via the coronary arteries during diastole3
- CoPP = DBP – LVEDP (left ventricular end-diastolic pressure)3
- Cerebral perfusion pressure (CPP): Pressure gradient to blood flow to the brain5
- CPP = MAP – ICP (Intracranial Pressure)5
- Tissue perfusion pressure (TPP): Defined as the difference between MAP and critical closing pressure (arterial pressure at which blood flow stops). Primarily used in critically ill, hemodynamically unstable patients.6
Intracardiac, Pulmonary, and Venous Pressures
Intracardiac Pressure
- Intracardiac pressure refers to the pressure within the four chambers of the heart used to assess cardiac function and evaluate for specific conditions.
- Intracardiac pressure can be obtained via Swan-Ganz catheterization.
Pulmonary Artery Pressure (PAP)
- PAP refers to the pressure against the walls of the pulmonary arteries generated by the contraction of the right ventricle.
- PAP can be used to identify pulmonary hemodynamics and identify conditions such as pulmonary hypertension.7
- PAP is obtained via catheterization or imaging like MRI/echocardiography.7
- Normal PAP values:
- Systolic: 15-28 mmHg
- Diastolic: 5-16 mmHg
- Mean PAP: 10-14 mmHg
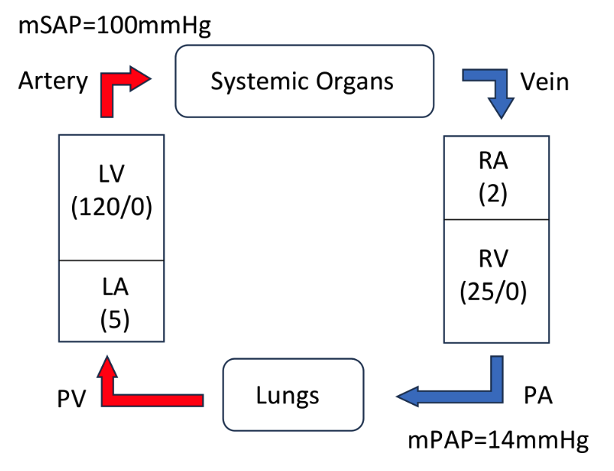
Figure 1. Schematic of intracardiac, pulmonary, and circulatory pressures. Abbreviations: LV, left ventricle; mSAP, mean systemic arterial pressure; LA, left atrium; RA, right atrium; RV, right ventricle; PA, pulmonary artery; mPAP, mean arterial artery pressure; PV, pulmonary vein.
Venous Pressure
- Venous pressure refers to the pressure of blood in the veins that return blood to the heart.
- It has two components: central and peripheral venous pressure
- Central venous pressure (CVP)
- CVP is the pressure measured in the superior vena cava near the right atrium.8
- CVP is primarily used as an indicator of venous return to the heart and a surrogate for right ventricular preload. This can be used to measure conditions such as volume, venous tone, and right heart function.8
- CVP is measured by placing a catheter into the internal jugular or subclavian veins. This can be seen on jugular venous pressure waveform graphs (Figure 2).8
- Jugular venous waveforms are identified as follows:
- a wave: Corresponds to right atrial contraction
- c wave: The bulging of the tricuspid valve into the right atrium during ventricular contraction
- x descent: Atrial relaxation and downward displacement of the tricuspid valve during ventricular contraction (systole)
- v wave: Atrial venous filling during a closed tricuspid valve
- y descent: Opening of the tricuspid valve to allow ventricular filling (diastole)8
- Jugular venous waveforms are identified as follows:
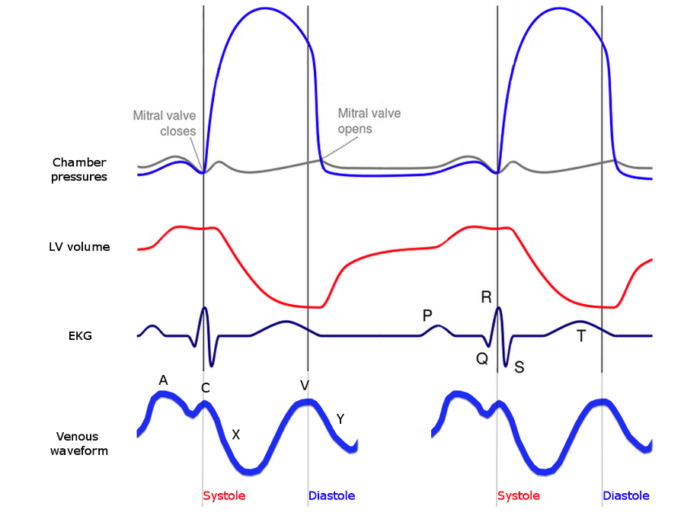
Figure 2. Wiggers diagram with jugular venous waveform. Source: Wikimedia Commons. 2018. Accessed 20 November 2024. Link Abbreviations: LV, left ventricle; EKG, electrocardiogram.
- Peripheral Venous Pressure (PVP)
- PVP is the pressure measured in distal peripheral veins.8
- PVP can be correlated with CVP and is measured via venous congestion plethysmography or ultrasound.8
Systemic Vascular Resistance and Viscosity
Systemic Vascular Resistance (SVR)
- SVR is the measure of total resistance created by all vasculature except the pulmonary vascular bed. SVR is calculated using the equation:9
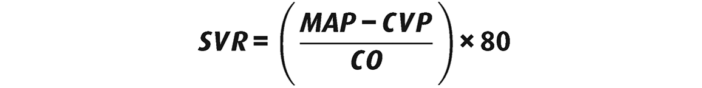
- SVR is analogous to left ventricular afterload and is influenced by many factors, including blood vessel diameter, vascular tone, and viscosity.9
- Elevated SVR can be seen in conditions like hypertension, cardiogenic shock, and a high hematocrit, while decreased SVR is seen in conditions such as anemia, anaphylaxis, and septic shock.9
Viscosity
- Viscosity, described as the internal friction of blood, is one of the main influencing factors of SVR and can impact blood flow through the vasculature.
- Poiseuille’s law dictates the relationship between viscosity and SVR:
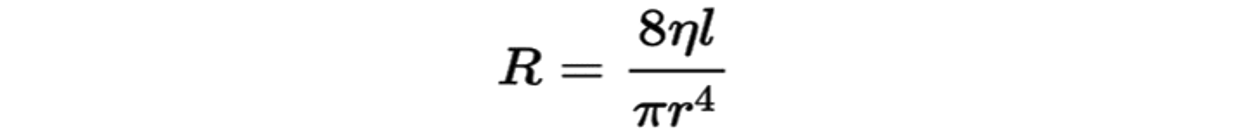
R = Resistance (SVR in this case)
n = viscosity
L = length of vessel
r = radius of vessel
- Viscosity depends on many factors, including hematocrit, plasma viscosity, and aggregability of red blood cells.10
- Due to its impact on SVR, increased viscosity can be associated with hypertension and atherosclerosis. Conditions such as cyanosis and accelerated erythropoiesis, sickle cell anemia, polycythemia vera, and Waldenstrom macroglobulinemia all can result in increased blood viscosity.10
Control of Arterial Blood Pressure
- Several immediate, intermediate, and long-term adjustments regulate arterial blood pressure.
- Minute-to-minute control of blood pressure – Baroreceptor reflex
- Intermediate control – Activation of renin-angiotensin-aldosterone system
- Long-term control – Renal mechanisms
Baroreceptor Reflex
- The baroreceptor reflex is the body’s response to maintaining homeostatic blood pressure.
- With elevated blood pressures (Figure 3): Baroreceptors located in the carotid sinuses and aortic arch detect high pressure → send afferent signals to the solitary nucleus in the brainstem via the glossopharyngeal and vagus nerves, respectively → brain stem (nucleus tractus solitarius in the medulla) sends output signals to increase parasympathetic activity and decreased sympathetic activity → vasodilation → decreased blood pressure, heart rate, stroke volume.
- With low blood pressures (Figure 3): Baroreceptors located in the carotid sinuses and aortic arch detect low pressure → send afferent signals to the solitary nucleus in the brainstem via the glossopharyngeal and vagus nerves, respectively → brain stem sends output signals to increase sympathetic activity and decreased parasympathetic activity → vasoconstriction → increased blood pressure, heart rate, stroke volume.
- In addition to baroreceptors detecting pressure homeostasis, peripheral chemoreceptors located nearby in the carotid and aortic bodies detect decreasing pH or PO2 or increasing pCO2. These bodies send signals via the glossopharyngeal and vagus nerves to stimulate the respiratory centers of the brain, increasing breathing and sympathetic outflow to the heart (Figure 3).
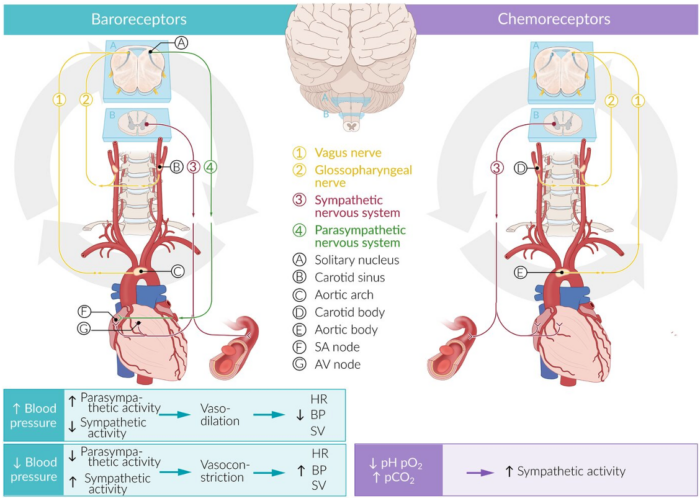
Figure 3. Baroreceptor and chemoreceptor pathways. Used with permission from Vascular Physiology. AMBOSS. Accessed 21 November 2024. Link
Intermediate and Long-term Control of BP
- This relies on the integration of neurologic signals transmitted via the parasympathetic and sympathetic components of the autonomic nervous system together with hormonal messaging controlled predominantly in the kidneys via the renin-angiotensinogen-aldosterone system.
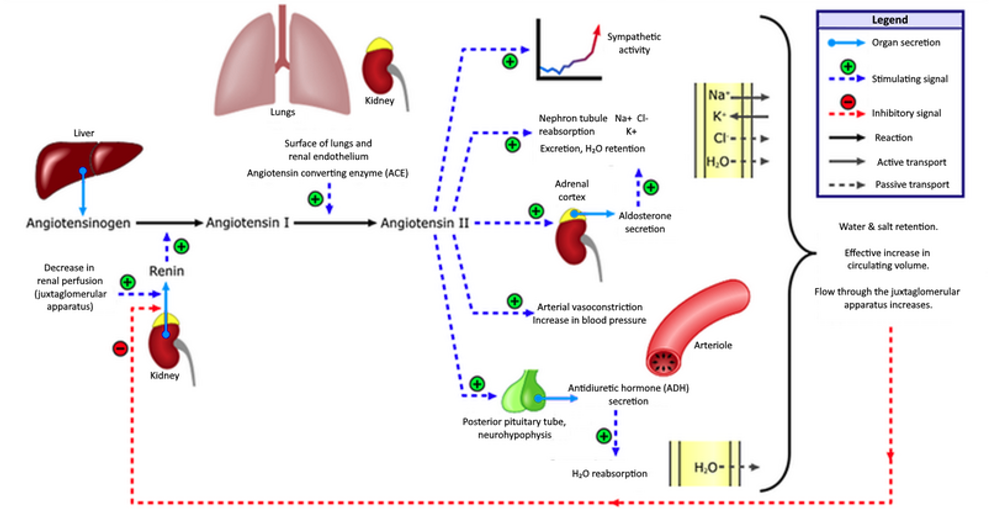
Renin-Angiotensinogen-Aldosterone System (RAAS)
- The RAAS system is the body’s main way of regulating intermediate and long-term blood pressure in response to fluid status, electrolyte levels, and renal perfusion.
- With decreased renal perfusion, electrolyte imbalances such as hyperkalemia and/or hyponatremia, dehydration, or sympathetic nervous system activation (Figure 4): The kidney releases renin via juxtaglomerular cells (stimulated via β1 receptors) → cleavage of angiotensinogen (produced by the liver) to angiotensin I → angiotensin I is cleaved by angiotensin-converting enzyme (ACE) in the lungs into angiotensin II.
- Angiotensin II is the main effector of the RAAS system and has a systemic range of effects, including:
- Arterial vasoconstriction to increase blood pressure
- Directly acts on the proximal convoluted tubule of the kidney to promote sodium, chloride and water retention with potassium excretion
- Stimulation of aldosterone synthesis and release from the adrenal cortex, which causes water and sodium retention and facilitates potassium excretion in the collecting ducts of the kidneys
- Stimulation of anti-diuretic hormone (ADH) release from the posterior pituitary, which increases water resorption in the late distal convoluted tubule and collecting ducts in the kidneys
References
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: Executive Summary: A report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Hypertension. 2018;71(6):1269-1324. PubMed
- McEvoy JW, Chen Y, Rawlings A, et al. Diastolic blood pressure, subclinical myocardial damage, and cardiac events: Implications for blood pressure control. J Am Coll Cardiol. 2016;68(16):1713-1722. PubMed
- Rosendorff C, Black HR, Cannon CP, et al. Treatment of hypertension in the prevention and management of ischemic heart disease: a scientific statement from the American Heart Association Council for High Blood Pressure Research and the Councils on Clinical Cardiology and Epidemiology and Prevention. Circulation. 2007;115(21):2761-2788. PubMed
- Gedde SJ, Vinod K, Wright MM, et al. Primary open-angle glaucoma preferred practice pattern®. Ophthalmology. 2021;128(1):P71-P150. PubMed
- Pelah AI, Czosnyka M, Menacho S, Nwachuku E, Hawryluk GWJ. Focal brain oxygen, blood flow, and intracranial pressure measurements in relation to optimal cerebral perfusion pressure. J Neurosurg. 2023;140(5):1423-1433. PubMed
- Chandrasekhar A, Padrós-Valls R, Pallarès-López R, et al. Tissue perfusion pressure enables continuous hemodynamic evaluation and risk prediction in the intensive care unit. Nat Med. 2023;29(8):1998-2006. PubMed
- Abman SH, Hansmann G, Archer SL, et al. Pediatric pulmonary hypertension: Guidelines from the American Heart Association and American Thoracic Society. Circulation. 2016;133(4):e368. PubMed
- Vlismas PP, Wiesenfeld E, Oh KT, et al. Relation of peripheral venous pressure to central venous pressure in patients with heart failure, heart transplant, and left ventricular assist device. Am J Cardiol. 2021;138:80-84. PubMed
- Lu DY, Fang Q, Bibby D, Arora B, Schiller NB. Association of systemic vascular resistance analog and cardiovascular outcomes: The Heart and Soul Study. J Am Heart Assoc. 2022;11(17):e026016. PubMed
- Nader E, Skinner S, Romana M, et al. Blood rheology: Key parameters, impact on blood flow, role in sickle cell disease, and effects of exercise. Front Physiol. 2019;10:1329. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.