Copy link
Barriers to Quality Improvement
Last updated: 07/11/2024
Key Points
- The Institute for Healthcare Improvement (IHI) sets quality goals that include efficient, safe, reliable, patient-centered, effective, and equitable care.
- Quality improvement (QI) is a science of methodical planning, multiple iterations, and interventions to yield improvements in a process or area. QI projects should follow a valid scientific method and attempt to monitor improvement over time and reflect sustainability.
- Deviation from the science or failure to follow the organization of a QI process may pose barriers to QI projects and improvement processes.1
- Team organization and planning are critical in improving processes and conducting a QI project.1
The Foundation of Process Improvement
- It is paramount to first understand the foundation of process improvement and how to plan a QI project following the Quality Improvement Methodology (Table 1). Straying from the basic QI methodology most commonly creates barriers.
- What is the goal of the improvement?
A SMART aim can address this by answering if the goal is Specific, Measurable, Attainable, Relevant, and Timebound.- Specific: The goal should be written and known to be specific to a particular area, group of patients, etc.
- Measurable: The goal should also be able to be measured by an objective score or designation of completion/incomplete, etc.
- Attainable: Formulating an unattainable goal may discourage teams, and it is unlikely that the project will be completed.
- Relevant: Understanding that the problem is truly an issue is helpful for leadership and team buy-in and for collecting baseline data to justify the need for a QI project initiation. It is important to analyze the problem by understanding a workflow or process through the construction of a process map.
- Timebound: To ensure that the project has an endpoint, a set period of time should be set as a goal to complete the project.
- Example of a clear SMART Aim: “This project aims to increase the percentage of patients who arrive on time for their scheduled clinic visits in the Rainbow Clinic from 40% to 65% by December 31st, 2024.”
- When a metric or data point set exists, it must be consistent so that all team members can read it without question. In this example, “arrive on time” should be further specified as “arrive at the check-in desk at Rainbow Clinic within 5 minutes of the scheduled time.” This specification is called an operational definition.
- One of the best ways to understand a process is to formulate a 5-7-step process map (Lean Six Sigma, Failure Mode Effects Analysis). Including various team members in the process ensures that it is understood and that all potential failures can be predicted for a proper prediction pattern. Failure to utilize a process map and misunderstanding a process can be a significant barrier to understanding the QI process.2
- How should a team be constructed?
- Understanding team members, leadership priorities, and how to influence others positively is crucial to project planning and ensuring that important considerations are made for all members of a process.
- The construction of a team with all appropriate members will help ensure a consensus on the problem at hand.
- If this project is not supported by stakeholders and leadership, it will be challenging to get buy-in for both resources and project planning to move this metric forward.
- What is the solution/intervention?
- If the solution is too large, initiating the intervention and initiating a small test of change (PDSA—Plan Do Study Act) can be challenging.
- By starting a project on a smaller scale (smaller group of patients, fewer operating rooms, fewer surgeons, etc.), one ensures that all minor issues/barriers are ironed out before spreading this to an entire system.
- While failures are likely to occur, smaller-scale failures or issues are more favorable than larger-scale issues, which may affect more people, patients, and team members.
- How do we determine an intervention or solution?
- When a solution or intervention for an ongoing issue involves more money, staff, or additional work created for an existing team member, this may pose apparent issues.
- If the intervention involves adding additional money or staff, leadership may hesitate unless a leadership team strongly drives this process.
- Considering how to automate or reframe job responsibilities may be favorable rather than adding to the existing requirements.
- How will the improvement be sustained?
- In an ideal scenario, the sustainability could be automated, or the plan may involve a longer-term shift in culture, for which the metric/outcome/process measure may not require monitoring if the data/numbers support that the process has been successful in a controlled environment for long enough.
- This may be determined by a run chart and a control chart, which shows that the process is in control and has minimized variability from the day-to-day process, as previously shown.
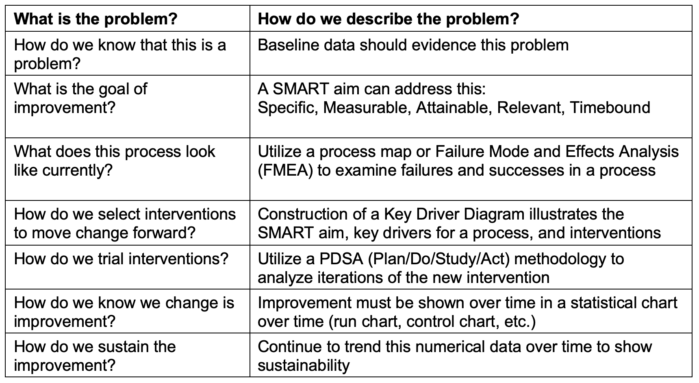
Table 1. Model for improvement questions to answer; Failure Mode and Effects Analysis -- Link; Key Driver Diagram -- Link; PDSA (Plan/Do/Study/Act) -- Link
- Table 2 illustrates barriers or problems encountered during project planning and their potential solutions.
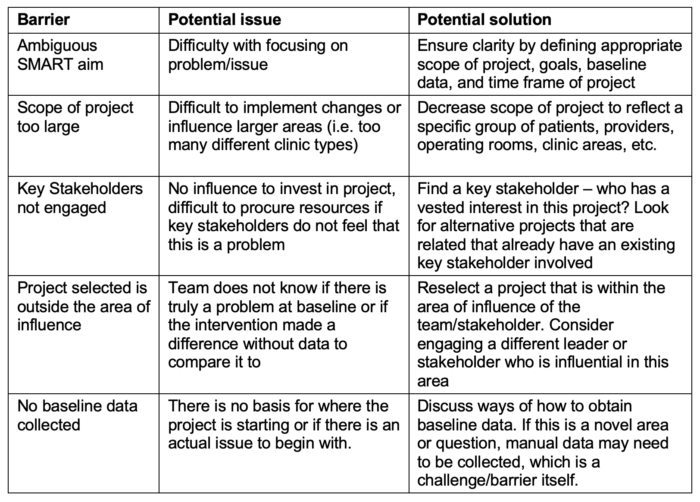
Table 2. Examples of project planning and barriers.
- Table 3 illustrates examples of barriers encountered after process creation.
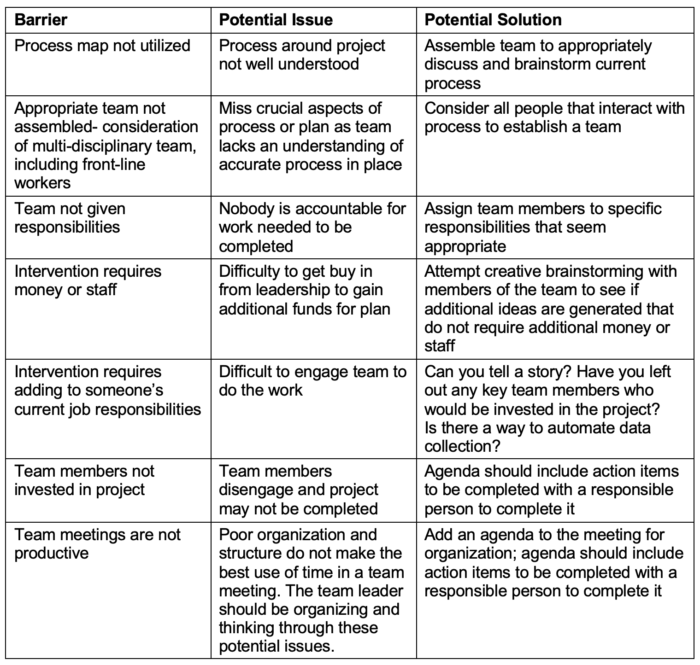
Table 3. Examples of barriers encountered after process creation
- Table 4 lists examples of barriers encountered after an intervention is in place.
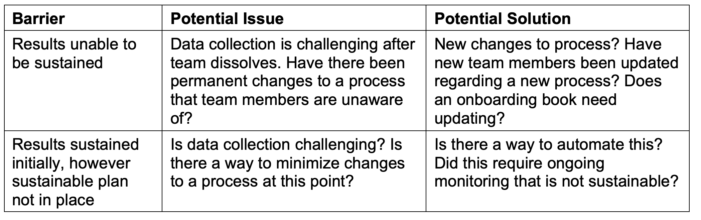
Table 4. Barriers after intervention are in place
References
- Scholtes PR, Joiner BL, Streibel BJ. Doing work as a team. In: The Team Handbook. Oriel Incorporated; 2003: 28 - 39. Accessed June 12, 2024. Link
- Langley GJ, Moen RD, Nolan, KM, et al. (2009). The Improvement Guide: A Practical Approach to Enhancing Organizational Performance. Germany: Wiley.
Other References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.