Copy link
Aortic Cross-Clamping
Last updated: 02/09/2024
Key Points
- An aortic cross-clamp is used during certain surgical procedures to stop blood flow temporarily.
- When the aortic cross-clamp is located more proximally in relation to the heart, there is an increased risk of myocardial ischemia and infarction, due to increased afterload and myocardial work.
- During aortic clamping, blood pressure should be kept high, to maintain collateral perfusion distal to the aortic cross-clamp.
- Measures to reduce hypotension after unclamping include the administration of fluids and vasopressors, as well as the slow removal of the aortic cross-clamp.
Indications
- The aorta is temporarily cross-clamped at the thoracic or abdominal levels during certain specific surgical procedures or during the management of severe trauma (Table 1).
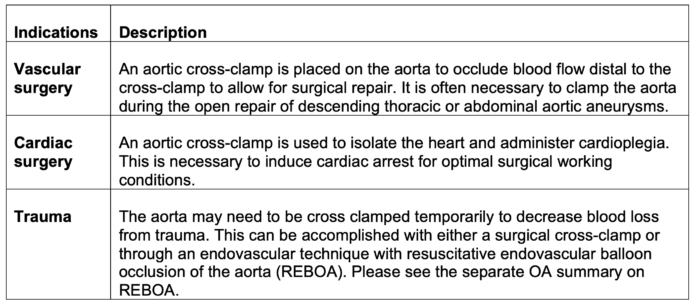
Table 1. Indications for aortic cross-clamping
Anatomy of the Aorta
- To understand pathophysiology of aortic cross-clamping, it is important to be familiar with the anatomy of the aorta and its branches (Figure 1).
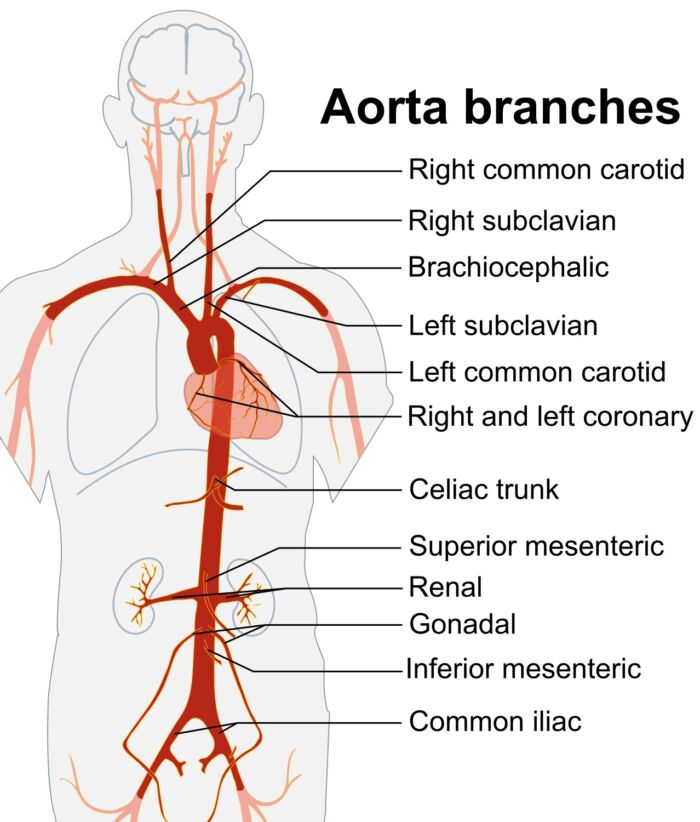
Figure 1. Branches of the aorta. Source: Wikimedia Commons. Mikael Hãggstrôm, based on work by Edoardado Marina Ruiz Villareal. CC BY SA 3.0. Link
Pathophysiology of Aortic Cross-clamping and Mechanisms of Ischemia
- The impact of the aortic cross-clamp on the development of ischemia depends on the duration of cross-clamp application, as well as the location of the cross-clamp.1,2
- An aortic cross-clamp time duration of greater than 90 minutes has been independently associated with higher mortality.1
- The pathophysiology of aortic cross-clamping is summarized in Figure 2.
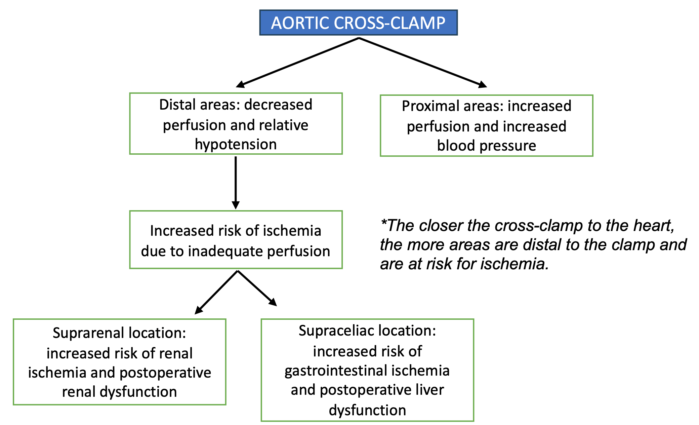
Figure 2. Pathophysiology of aortic cross-clamping
Hemodynamic Changes with Aortic Cross-Clamping
In general, the hemodynamic changes with aortic cross-clamping are as follows (Figure 3).
- Hypertension due to increased afterload from impedance to aortic blood flow, increased myocardial contractility due to catecholamine and vasoconstrictor release, and maintenance of cardiac performance.1
- Blood volume redistribution, and hence preload, depends on the level of the cross-clamp1 (Figure 4). During supraceliac aortic cross-clamping, the shift of blood volume from areas distal to the clamp to areas proximal to the clamp increases the preload. However, during infraceliac aortic clamping, the blood volume may redistribute to the splanchnic circulation instead without an increase in preload. This distribution of blood volume between the heart and splanchnic vasculature depends on the overall sympathetic tone.1
- Increases in afterload and preload result in an increase in contractility and myocardial oxygen demand, with an increase in coronary blood flow in normal circumstances. However, in the event of the inability of the myocardium to increase contractility and /or coronary blood flow, the cardiac output decreases.1
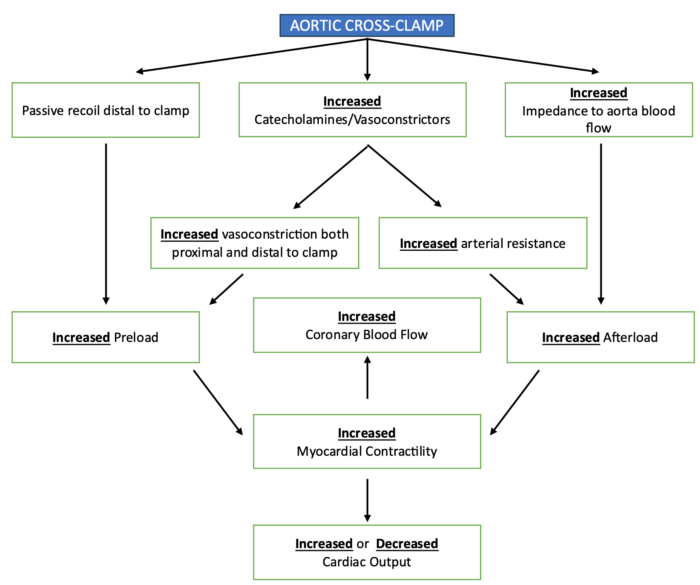
Figure 3. Hemodynamic changes with aortic cross-clamping. Adapted from Gelman S. The pathophysiology of aortic cross-clamping and unclamping. Anesthesiology 1995;82(4):1026-60.2
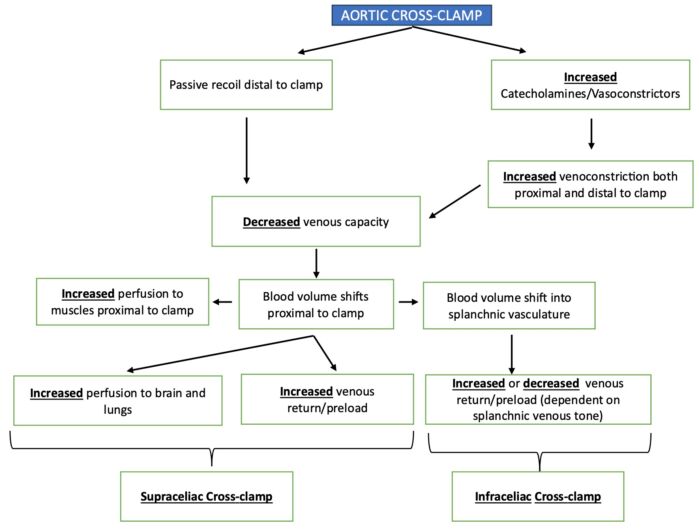
Figure 4. Blood volume redistribution with aortic cross-clamping. Adapted from Gelman S. The pathophysiology of aortic cross-clamping and unclamping. Anesthesiology 1995;82(4):1026-60.2
Humoral Effects of Cross-Clamping
During aortic cross-clamping, several vasoactive substances and mediators are released, altering blood flow and hemodynamic parameters.1,2
Acidosis
- Acidosis and increased lactate levels develop in the ischemic areas distal to the aortic cross-clamp.1,2
- Longer duration of cross-clamping result in a larger increase in acidosis and lactate levels.
- Acidosis and the release of inflammatory mediators in distal areas result in distal volume expansion and hypotension from loss of preload.
- Sodium bicarbonate administration does not prevent hypotension, likely because it does not correct acidosis in the tissues, including the arterial walls.2
- With unclamping, CO2 level rises due to washout of distal tissues and from increased production due to the inflammation from re-perfusion.2
Renin-Angiotensin System
- Renin and angiotensin levels both increase during cross-clamping.1,2
- Suprarenal clamping results in decreased perfusion to the afferent arterioles of the kidney resulting in increased production of renin and angiotensin.1,2
- Increased levels of the same also are seen in infrarenal clamping, for unclear reasons.
- Despite, persistence of these hormone levels for hours after clamp removal, they have not been shown to result in hypertension.
Catecholamines
- During cross-clamping, epinephrine and norepinephrine levels increase, and the etiology for this increase is multifactorial.1,2
- Epinephrine is predominantly released during the application of the cross-clamp, while norepinephrine is primarily released when the clamp is removed.1,2
- Sympathetic activation from ischemia and hypotension likely contribute to these findings.
Reactive Oxygen Species
- Ischemia-reperfusion results in the production of reactive oxygen species, which can cause tissue damage and organ dysfunction.1,2
Phosphate
- Reperfusion of ischemic tissues results in increased production of phosphate containing compounds, leading to a shift in phosphate from the extracellular to the intracellular compartment.1,2
- For at least 48 hours after a cross-clamp is used, phosphate repletion may be necessary.
Cytokines and Other Inflammatory Mediators
- The ischemia from aortic cross-clamping results in increased production of inflammatory mediators such as tumor necrosis factor (TNF) and Interleukin 6 (IL-6).1,2
- The impact of these mediators is not completely clear, but TNF is associated with lung injury after reperfusion.
Hemodynamic effects/Pathophysiology of Aortic Unclamping
- Unclamping of the aorta is associated with substantial decreases in vascular resistance and arterial blood pressure (Figure 5).
- The main reasons for hypotension following unclamping include1,2
- central hypovolemia due to increased venous capacitance and pooling of blood distal to the clamp.
- arterial vasodilation due to decreased arterial resistance.
- accumulation of metabolites with myocardial depressant and vasoactive properties.
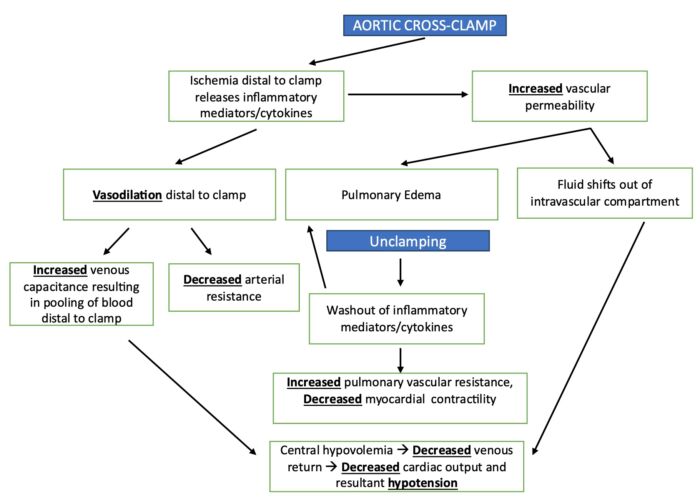
Figure 5. Impact of removal of aortic cross-clamp. Adapted from Gelman S. The pathophysiology of aortic cross-clamping and unclamping. Anesthesiology 1995;82(4):1026-60.1
Preparation Prior to Cross-Clamp Removal
- Several steps can be taken to reduce the negative hemodynamic effects of aortic unclamping (Table 2).
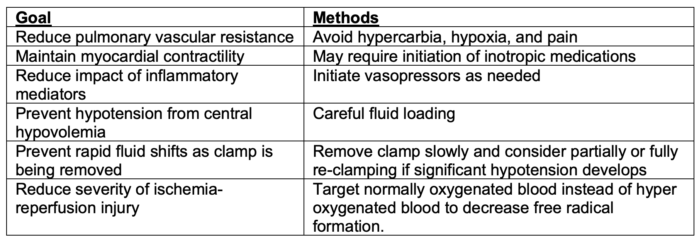
Table 2. Strategies to reduce the negative hemodynamic effects of aortic unclamping
References
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.