Copy link
Alcohol Abuse
Last updated: 09/18/2024
Key Points
- Alcohol use disorder (AUD) is the most commonly diagnosed substance use disorder.
- AUD has been shown to increase postoperative morbidity.
- Alcohol withdrawal is a potentially life-threatening condition that should be treated with long-acting benzodiazepines.
Introduction
- The prevalence of alcohol use disorder (AUD) in the United States is estimated to be 29.5 million among people older than 12 years and is the most commonly diagnosed substance use disorder, with 23.5% of adults (18 years and older) reporting binge drinking in the past month, and 6.3% reporting heavy alcohol use.1
- Given the prevalence, it is essential to consider how alcohol consumption impacts organ systems and chronic disease states, as well as considerations for perianesthetic management.
Effects of Ethyl Alcohol on Organ Systems
Neuropsychiatric Effects
- Acute abuse
- Wernicke encephalopathy: Wernicke encephalopathy is due to thiamine deficiency. Patients present with ataxia, oculomotor abnormalities, and altered mental status.2
- Seizure/hallucinosis/delirium tremens: See “Alcohol Withdrawal Syndrome” below.
- Chronic abuse
- Korsakoff syndrome: Korsakoff syndrome is due to untreated thiamine deficiency. It is characterized by anterograde and retrograde amnesia.2
- Dementia: Alcohol abuse likely contributes to the development of dementia due to glutamate neurotoxicity and impaired neural regeneration.3
- Peripheral neuropathy: Long-term thiamine deficiency causes nerve damage.1
- Cerebellar degeneration: Cerebellar degeneration causes irreversible gait and coordination difficulties due to direct toxicity from alcohol and thiamine deficiency.3
Cardiovascular
- Acute abuse
- Holiday heart syndrome: Holiday heart syndrome describes the onset of atrial fibrillation (AFib) after binge drinking. Alcohol promotes cardiac arrhythmias due to thickening of connective tissue, electrolyte disturbances, decreased myocardial oxygen delivery, and increased plasma levels of catecholamines.4
- Chronic abuse
- Hypertension: Alcohol is a known modifiable risk factor for hypertension (HTN) and cardiovascular disease.3
- Cardiomyopathy: Alcohol-induced cardiomyopathy accounts for approximately one-third of dilated cardiomyopathy cases. Alcohol is thought to cause cardiac myocyte apoptosis, decreased synthesis of contractile protein, and decreased cardiac output.3
- Arrhythmias: AFib incidence increases with alcohol consumption in a dose-dependent manner. Alcohol causes direct damage and oxidative stress to atrial myocytes. Inflammation can result in atrial remodeling and fibrosis.3
- Stroke: Heavy alcohol consumption precipitates ischemic strokes due to blood clots. Embolic strokes have been attributed to AFib and alcoholic cardiomyopathy. HTN may put patients at higher risk of hemorrhagic stroke.4
Respiratory
- Respiratory depression: Acute alcohol intoxication can cause respiratory depression. Anesthesiologists should ensure intoxicated patients can protect their airways.2
- Respiratory infections: Patients with AUD have impaired immune integrity, glottic reflexes, and mucociliary function, putting patients at higher risk of aspiration and pneumonia.3
Gastrointestinal (GI)
- Alcoholic liver disease: Alcoholic liver disease is a spectrum of diseases.
- Alcoholic fatty liver: Fat accumulation in the liver parenchyma secondary to the effects of alcohol abuse.5
- Alcoholic hepatitis: Alcoholic hepatitis is defined by the onset of jaundice within 60 days of heavy alcohol use, serum bilirubin >3 mg/dL, elevated aspartate aminotransferase (AST), AST: alanine aminotransferase (ALT) ratio >1.5, and no other cause of acute hepatitis. Liver injury occurs due to lipogenesis and inflammation in hepatocytes.5
- Cirrhosis: Cirrhosis is irreversible liver damage characterized by hepatic fibrosis and loss of liver function. Cirrhosis complications include portal HTN, esophageal varices, coagulopathy, and hepatocellular carcinoma.5
- Gastritis: Alcohol consumption increases gastric acid production, promoting gastritis.3
- Upper GI bleeding
- Mallory-Weiss tear: With chronic retching and vomiting, patients can develop tears in the mucosa of the gastroesophageal junction, resulting in painful bleeding.3
- Peptic ulcer disease: Alcohol upregulates gastric acid production, which may cause ulcer formation and bleeding.3
- Esophageal varices: Varices result from portal HTN, putting patients at high risk of bleeding and impaired airway visualization.3
- Esophagitis: Alcohol reduces lower esophageal sphincter pressure and promotes esophageal dysmotility, increasing the risk for gastroesophageal reflux disease.3
- Pancreatitis
- Acute: Alcohol-induced acute pancreatitis is likely due to a combination of direct toxicity of alcohol to acinar cells and environmental/genetic factors.3
- Chronic: Alcohol is attributed to 60% to 90% of chronic pancreatitis cases.3
Renal
- Alcoholic ketoacidosis: Alcoholic ketoacidosis is often the result of poor nutritional intake in the setting of vomiting and nausea. An anion-gap metabolic acidosis forms from fatty acid oxidation, resulting in the accumulation of ketoacids.6
- Hyponatremia: Hyponatremia is due to the increased release of vasopressin in the setting of volume depletion and increased risk of osmotic demyelination.6
- Hypophosphatemia: Hypophosphatemia is primarily attributed to poor intake but also due to renal loss from alcohol-induced tubular dysfunction and decreased GI uptake.6
- Hypomagnesemia: Hypomagnesemia is promoted by GI losses and alcohol-induced renal tubular dysfunction.6
- Hypocalcemia: Hypocalcemia worsens in the setting of hypomagnesemia settings (low magnesium → low parathyroid hormone). Other causes include urinary loss and vitamin D deficiency.6
- Hypokalemia: Hypokalemia occurs in the setting of inadequate intake, increased aldosterone release in the setting of dehydration, and diarrhea.6
Endocrine
- Osteoporosis: Alcohol use is associated with deficiencies in vitamin D, osteocalcin, and insulin-like growth factor 1. In patients with AUD, osteoporosis fractures are more common.3
- Hypothyroid: Hypothyroidism in AUD occurs because of decreased peripheral thyroid hormones and decreased response to thyroid-stimulating hormone from direct thyroid toxicity.3
Hematologic
- Impaired immunity: Alcohol use decreases the number and impairs the function of B and T cells, predisposing patients to bacterial and viral infections. Patients with AUD have an increased incidence of pulmonary infections, human immunodeficiency virus, hepatitis B and C, and other sexually transmitted infections.3
- Anemia: Chronic alcoholism reduces blood cell precursors in the bone marrow.7 Alcoholics may develop anemia due to vitamin B deficiencies.
- Coagulopathy:
- Thrombocytopenia: Patients usually do not exhibit excessive bleeding. Most patients return to baseline after one week of alcohol cessation (if there is no underlying liver disease).7
- Thrombocytopathy: Alcohol impacts platelet aggregation, decreases secretion/activity of proteins involved in clotting, and prolongs bleeding time. Alcohol can interact with common anticoagulants, increasing the risk of bleeding.7
Musculoskeletal
- Rhabdomyolysis: Sudden decreases in plasma phosphate levels in patients who binge drink can cause acute rhabdomyolysis.6
Malignancy
- Alcohol consumption carries a dose-related risk of oropharyngeal, esophageal, gastric, breast, colorectal, hepatocellular, and pancreatic cancers.1
Nutritional Deficiencies
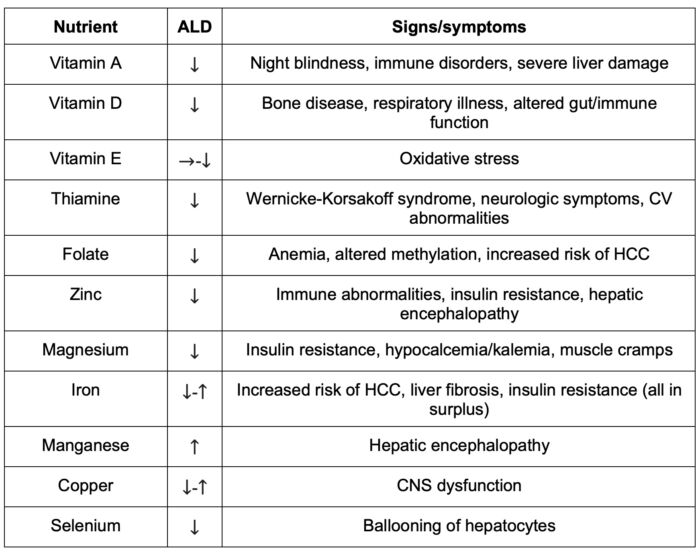
Table 1. Deficiency or surplus of vitamins, major minerals, and trace elements in ALD. Adapted from Masaki et al.8 Abbreviation: ALD, alcoholic liver disease; CNS, central nervous system; CV, cardiovascular; HCC, hepatocellular carcinoma.
Anesthetic Considerations
AUD increases postoperative morbidity and higher rates of readmission to the intensive care unit.9
Preoperative Considerations
- Neurological: Anxiety and tremulousness are early indicators of alcohol withdrawal.9
- Cardiovascular: Preoperative electrocardiogram and echocardiogram can provide information about cardiac function, arrhythmias, and chronic cardiac changes.9
- Respiratory: Patients should be screened for lung pathology. A chest X-ray is recommended.1
- GI: Rapid sequence intubation should be considered in acutely intoxicated patients or chronic misusers due to increased risk of aspiration and delayed gastric emptying. Liver function tests can identify hypoalbuminemia or coagulopathy. An AST: ALT ratio of >2 suggests alcoholic liver disease, and elevated gamma-glutamyl transferase suggests chronic alcohol misuse.9
- Musculoskeletal: Patients should be examined for neuropathies and myopathies.9
- Heme: Complete blood count to evaluate for thrombocytopenia and anemia.1
- Nutrition: Patients with chronic heavy alcohol use should be given intravenous/intramuscular thiamine (100 mg/day for 3-5 days) and assessed for electrolyte abnormalities that should be corrected before elective surgery.9
Intraoperative Considerations
- Inhalational agents: No studies suggest a superior inhalational agent.1
- With acute intoxication, the minimum alveolar concentration (MAC) of inhalational agents is reduced by 40% or more, depending on the blood alcohol level.
- With chronic use, the MAC of inhalational agents is increased.
- Hypnotics:
- With acute intoxication, there is an increased sensitivity to barbiturates, benzodiazepines, and opioids.
- Patients with chronic use may require higher anesthetic doses due to enzyme induction and cross-tolerance.
- Hypnotic agents should be used according to the patient’s clinical condition. Cardiovascular-stable patients can tolerate propofol. If the patient is hemodynamically unstable or has alcohol-induced cardiomyopathy, etomidate is suggested. When severe hypotension or hemodynamic instability is present, ketamine is an option.9
- Neuromuscular blockers (NMBs): Cirrhotic patients may require higher doses of NMBs due to increased volume of distribution. NMBs with minimal or nonhepatic metabolism (e.g., atracurium, cisatracurium) are advisable. In severe liver failure, serum plasma cholinesterase levels may be decreased, resulting in a longer duration of action of succinylcholine.9
- Opiates: Most opiates are well tolerated; however, remifentanil is most desirable in patients with liver disease as it exhibits organ-independent metabolism and elimination.9
- Hemodynamics: Acute intoxication disrupts the autonomic nervous system, resulting in hypotension.9
Postoperative Considerations
- Patients who tolerate intraoperative anesthesia generally have uneventful postoperative courses. Postoperative complications in patients with alcohol misuse include bleeding, infection, cardiac dysfunction, and impaired cognitive function.9
- Patients in recovery: Perioperative exposure to sedatives or opioids may increase cravings or relapse. Use opioid-sparing pain management approaches where possible; however, opioids should be used when clinically indicated.10 Acetaminophen administration is safe when limited to no more than 4 grams per day.11
Alcohol Withdrawal Syndrome
Pathophysiology
- Normally, inhibitory (gamma-aminobutyric acid [GABA]) and excitatory (glutamate) signals are balanced (Figure 1).12
- Alcohol is a central nervous system depressant that facilitates GABA signaling. Over time, GABA receptors are downregulated, and glutamate receptors are upregulated in compensation (Figure 1c). Acute alcohol use decreases anesthetic requirements.12
- During alcohol withdrawal, there is a relative excess of excitatory signaling. This results in tachycardia, HTN, diaphoresis, tremulousness, delirium, and seizures (Figure 1d). Thus, chronic alcohol substance abuse increases anesthetic requirements.12
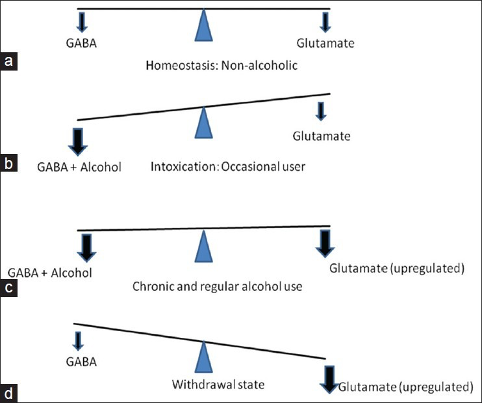
Figure 1. Neurochemistry of alcohol withdrawal. Source: Kattimani S, et al. Clinical management of alcohol withdrawal: a systematic review. Ind Psychiatry J. 2013.12 CC BY NC SA 3.0
Timeline of Symptoms
- Six hours after the last drink: Minor withdrawal symptoms begin, characterized by tremors, sweating, tachycardia, GI upset, headache, and anxiety. Patients are at the highest risk of withdrawal seizures in this time period. This phase lasts approximately 24-48 hours.12
- Twenty-four hours after the last drink: Alcoholic hallucinosis may be present, characterized by visual, tactile, or auditory hallucinations. This phase lasts up to 6 days.1
- 48-72 hours after last drink: Patients are at the highest risk of delirium tremens, characterized by tremors, sweating, anxiety, tachycardia, hallucinations, disorientation, and agitation. Delirium tremens may last up to 2 weeks.12
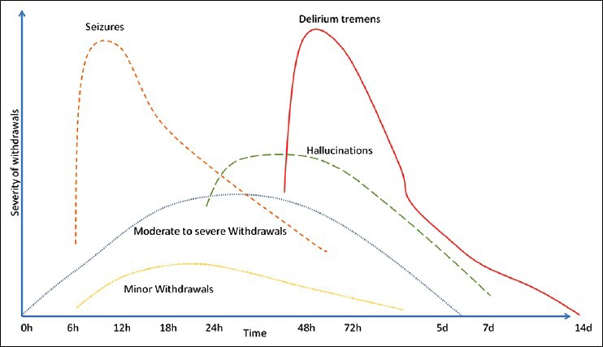
Figure 2. Time course of alcohol withdrawal symptoms. Source: Kattimani S, et al. Clinical management of alcohol withdrawal: a systematic review. Ind Psychiatry J. 2013.12 CC BY NC SA 3.0
Diagnosis
- Alcohol withdrawal syndrome is a clinical diagnosis based on patient history and physical exam.12
- The severity of symptoms can be determined with the Clinical Institute Withdrawal Assessment (CIWA) scoring to guide treatment. The CIWA score is a quantification of the severity of these withdrawal symptoms: agitation, anxiety, auditory disturbances, clouding of sensorium, headache, nausea/vomiting, paroxysmal sweats, tactile disturbances, tremors, and visual disturbances.12
Treatment
- Symptom-triggered treatment: Symptom-triggered treatment is driven as per the CIWA protocol. A long-acting benzodiazepine is administered when the CIWA score is >8.12
- Fixed dose: Fixed-dose treatment administers a fixed daily dose of benzodiazepines based on an estimate of the patient’s alcohol consumption.12
- Loading dose: Loading-dose strategies use long-acting benzodiazepines for their self-tapering effect (e.g., diazepam). CIWA scores and the patient’s clinical condition are considered before each dose.12
References
- Nehring SM, Chen RJ, Freeman AM. Alcohol use disorder. In: StatPearls [Internet]. StatPearls Publishing; 2024. Accessed July 23, 2024. Link
- LaHood AJ, Kok SJ. Ethanol toxicity. In: StatPearls [Internet]. StatPearls Publishing; 2023. Accessed July 23, 2024. Link
- Abbas D, Ciricillo JA, Elom HA, Moon AM. Extrahepatic health effects of alcohol use and alcohol-associated liver disease. Clin Ther. 2023;45(12):1201-11. PubMed
- Zakhari S. Alcohol and the cardiovascular system. Alcohol Health Res World. 1997;21(1):21-9. PubMed
- Patel R, Mueller M. Alcoholic liver disease. In: StatPearls [Internet]. StatPearls Publishing; 2023. Accessed July 23, 2024. Link
- Palmer BF, Clegg DJ. Electrolyte disturbances in patients with chronic alcohol-use disorder. N Engl J Med. 2017;377(14):1368-77. PubMed
- Ballard HS. The hematological complications of alcoholism. Alcohol Health Res World. 1997;21(1):42-52. PubMed
- Tadokoro T, Morishita A, Himoto T, et al. Nutritional support for alcoholic liver disease. Nutrients. 2023;15(6):1360. PubMed
- Fox CJ, Liu H, Kaye AD. The anesthetic implications of alcoholism. Int Anesthesiol Clin. 2011;49(1):49-65. PubMed
- May JA, White HC, Leonard-White A, et al. The patient recovering from alcohol or drug addiction: special issues for the anesthesiologist. Anesth Analg. 2001;92(6):1601-8. PubMed
- Bartels S, Sivilotti M, Crosby D, Richard J. Are recommended doses of acetaminophen hepatotoxic for recently abstinent alcoholics? A randomized trial. Clin Toxoicol (Phila). 2008;46(3):243-9. PubMed
- Kattimani S, Bharadwaj B. Clinical management of alcohol withdrawal: a systematic review. Ind Psychiatry J. 2013;22(2):100-8. PubMed
Other References
- The Alcohol Use Disorders Identification Test- Concise (AUDIT-C) is a brief alcohol screening instrument that identifies persons who are hazardous drinkers or have active alcohol use disorders (including alcohol abuse or dependence). Link
- NIAAA Healthcare Professional’s Core Resource on Alcohol. Link
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.