Copy link
Acute Liver Failure
Last updated: 09/11/2024
Key Points
- Acute liver failure (ALF) is a life-threatening acute liver illness or injury characterized by severely impaired hepatic dysfunction, which must include encephalopathy, in a patient without a history of pre-existing liver disease.
- To be considered true ALF, the deterioration from normal function must occur in less than 26 weeks.
- Supportive management should be administered in a center capable of transitioning care to organ transplantation if necessary.
- Liver transplantation (LT) may be the only treatment in advanced disease where supportive measures have failed.
Introduction
- The most common cause of ALF in the USA and Europe is acetaminophen toxicity.1 In developing nations, ALF is usually a result of one of many viral infections (Table 1).
- The incidence of ALF in developed countries has been reported at 1-6 cases per million population per year.2
- ALF is associated with large-scale hepatic necrosis with dramatically reduced metabolic and synthetic activity, resulting in widespread physiological derangement and, ultimately, multiorgan failure.
- Although the definition of ALF suggests an absence of pre-existing liver disease, there are several conditions where advanced fibrosis may exist in an otherwise normally functioning liver (e.g., Wilson disease, Budd-Chiari syndrome, reactivation of chronic hepatitis B viral infection, and autoimmune hepatitis) and failure may present in a hyperacute or “fulminant” fashion.
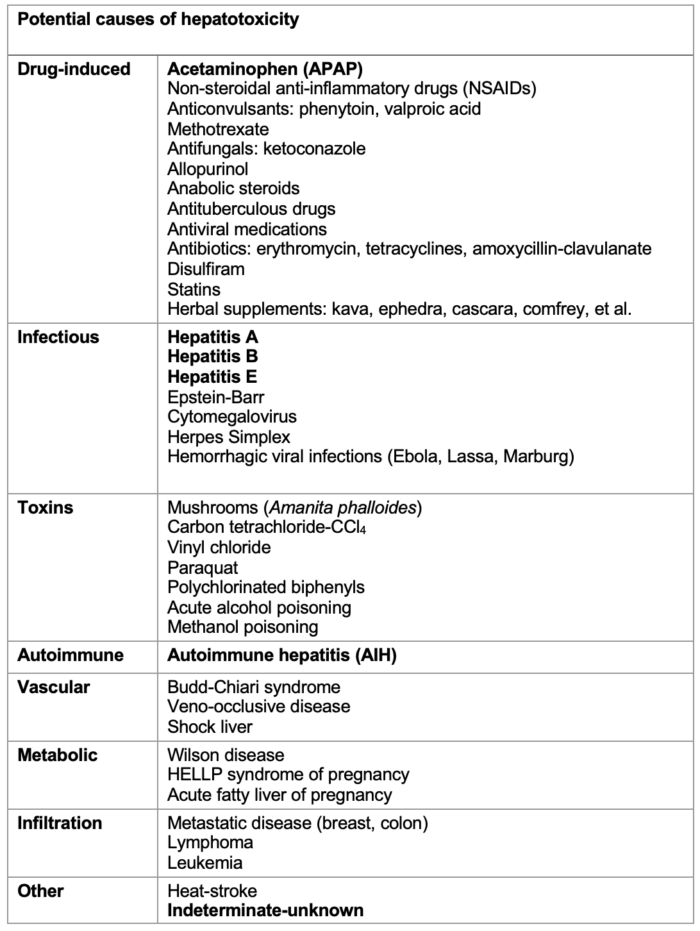
Table 1. Causes of liver toxicity which may progress to ALF. The most frequent are in bold font, with acetaminophen being the most common cause in developed nations and viral infections in developing nations. The list is not exhaustive. In some cases, the cause is undetermined.
Diagnosis
- It is important to obtain a comprehensive history early in the presentation, given that encephalopathy can progress to the point where it may not be possible to ask the patient due to a deteriorating mental state. Information should be sought specifically regarding:
- underlying health conditions;
- recent surgical or anesthetic interventions;
- full drug history, including use of herbal supplements;
- timeline for deterioration;
- alcohol use history; and
- mental health assessment.
- It is important to differentiate ALF from acute-on-chronic liver failure as the management can be very specific for each of the different causes, and the decision whether to progress to LT can be affected.
- Bedside examination usually reveals altered mental status, abdominal pain (usually right upper quadrant), hypotension, jaundice, and a low-grade fever. Peripheral edema may also be present. Signs of portal hypertension (ascites, varices, caput medusa) may not be present.
- Liver function tests usually reveal marked transaminitis and hyperbilirubinemia.
- Hemoglobin levels and platelet counts are often reduced.
- Screening tests on urine and blood must be performed, looking for drugs, toxins, and alcohol.
- Liver imaging using Doppler ultrasound is used to assess portal blood flow (Budd-Chiari syndrome) and detect cirrhosis.
- Liver biopsies to aid diagnosis may be deemed too high-risk in coagulopathic patients but can be performed on the explanted organ if LT is undertaken.
Clinical Features
- Hepatic encephalopathy is one of the defining features of ALF.2 The pathophysiology is multifactorial but hyperammonemia from the failure to convert ammonia to urea, raised glutamate levels, circulating inflammatory mediators, and a leaky blood-brain barrier play their part.
- Acute kidney injury is present in 30-70% of patients. Renal replacement therapy may be needed to maintain acid-base and biochemical homeostasis.
- Lung involvement (pulmonary edema or infections) is found in 30% of patients.
- The presence of coagulopathy reflects severely impaired liver synthetic function. The INR is necessarily prolonged (as in the definition, >1.5), but the bleeding risk is more accurately assessed using viscoelastic testing.
- There is a high incidence of bacterial and fungal infections, necessitating the possible use of prophylactic antimicrobials.
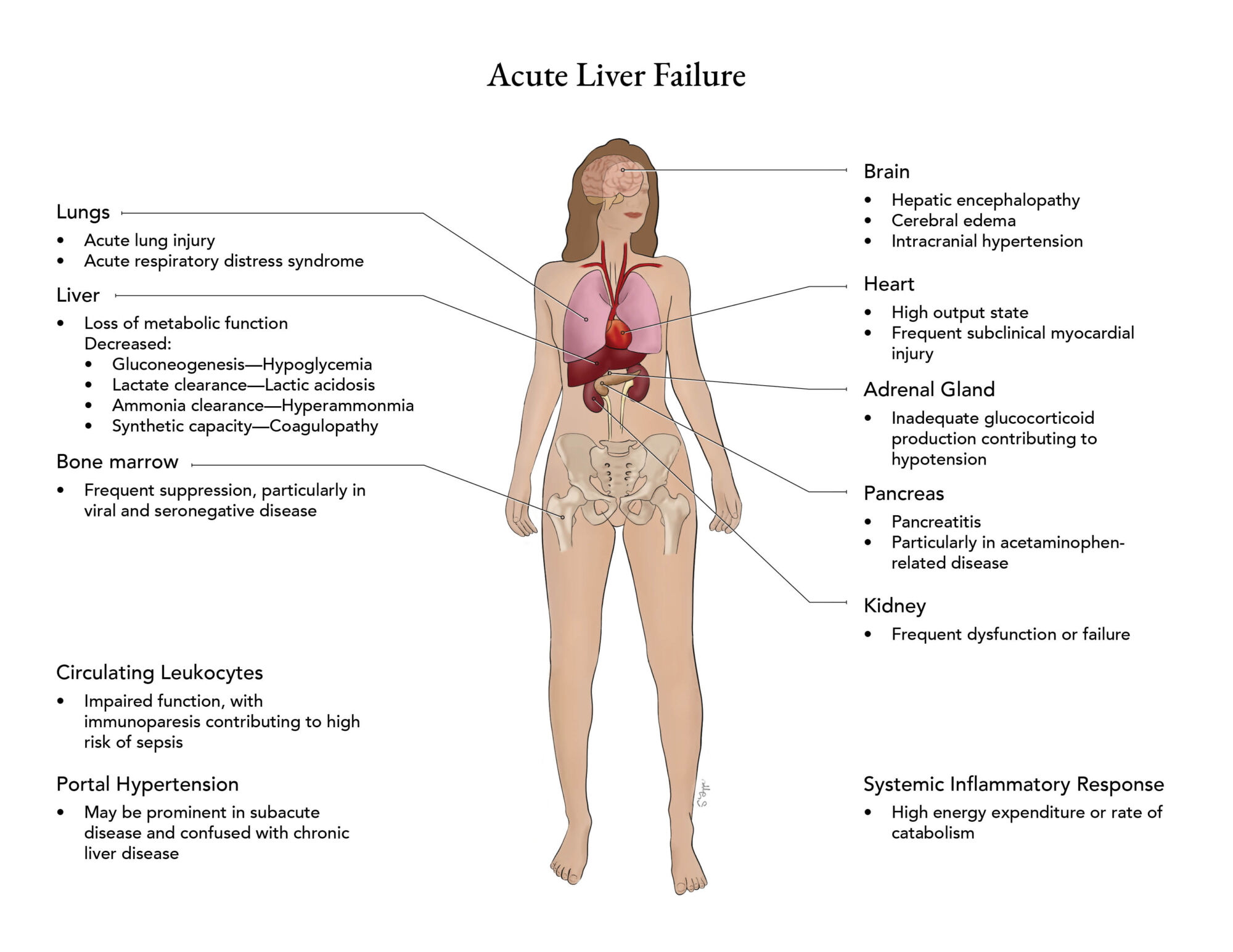
Figure 1: Clinical features of ALF highlighting the multisystem nature of the condition. Adapted from Bernal W, Wendon J. Acute liver failure. N Engl J Med. 2013; 369:2525-2534
Treatment Options
- Because ALF is relatively rare, evidence-based recommendations for care are lacking.3
- Cardiovascular: Initial treatment is supportive and focused on maintaining end-organ perfusion and oxygen delivery. Patients frequently have systemic and splanchnic vasodilation similar to that seen in sepsis, and vasopressor use is the basis for treatment. Norepinephrine, with the addition of vasopressin, is the medication of choice.
- Respiratory: Early endotracheal intubation may be necessary to protect the airway as the patient’s mental status deteriorates and to facilitate hyperventilation to maintain hypocarbia in the presence of developing cerebral edema.
- Neurological: Patients are usually sedated in the intensive care unit and nursed in a head-up position. Maintaining normothermia and normoglycemia is important. Noninvasive cerebral monitoring (transcranial Doppler) is preferred over invasive (intracranial pressure monitoring device).
- Renal: Early utilization of continuous renal replacement therapy should occur to reduce hyperammonemia to <100 mmol/L, along with the correction of other electrolyte and acid-base disturbances.3
- Gastrointestinal: Early enteral feeding should be started along with stress ulcer prophylaxis.
- Sepsis: It is common for infections to be present or develop, so surveillance and prophylaxis should be considered.4
- Coagulation: Once again, regular testing should be employed. But, in the absence of actual bleeding or a risk of bleeding during procedures, aggressive correction should not be undertaken. Plasma exchange has been utilized with some beneficial effects, especially in cases where LT is not considered a viable option, but also as a bridge to LT.4
- When ALF progresses rapidly, cerebral edema is more likely to develop. When the progression is slower, portal hypertension and associated problems become more common.
- As cerebral edema worsens, the rise in intracranial pressure can lead to brainstem herniation and death.
- Specific treatments for known etiologies3,5
- Acetaminophen hepatotoxicity (AH): In patients with AH, the time interval from ingestion to the administration of N-acetylcysteine (NAC) is closely related to outcome. Activated charcoal should be used for gastric decontamination as soon as poisoning is suspected.
- Nonacetaminophen hepatotoxicity (NAH): NAC may also play a role in NAH, and corticosteroids may also be effective if the disease has hypersensitivity or autoimmune features.
- Viral disease: If viral hepatitis is suspected, the appropriate antivirals should be started as soon as possible, although overall management of the ALF remains supportive in nature.
- Budd-Chiari syndrome: anticoagulation therapy should be started, and the patient should be considered for placement of a transjugular intrahepatic portosystemic shunt.
Outcomes
- Approximately 50% of patients with ALF eventually undergo LT with a one-year survival rate of around 80%.6
References
- Stravitz R, Lee W. Acute liver failure. Lancet. 2019; 394(10201):869-81. PubMed
- Bernal W, Wendon J. Acute liver failure. N Engl J Med. 2013;369(26):2525-34. PubMed
- Nanchal R, Subramanian R, Karvellas C, et al. Guidelines for the management of adult acute and acute-on-chronic liver failure in the ICU: Cardiovascular, endocrine, hematologic, pulmonary, and renal considerations. Crit Care Med. 2020;48(3):e173–e191. PubMed
- European Association for the Study of the Liver. Clinical Practice Guidelines Panel. EASL Clinical practical guidelines on the management of acute (fulminant) liver failure. J Hepatol 2017; 66:1047–81. PubMed
- Chris-Olaiya A, Kapoor A, Ricci K. Therapeutic plasma exchange in liver failure. World J Hepatol. 2021;13(8): 904-15. PubMed
- Olivo R, Guarrera J, Pyrsopoulos N. Liver transplantation for acute liver failure. Clin Liver Dis. 2018;22(2):409–17. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.