Copy link
Interscalene Block
Last updated: 03/07/2025
Key Points
- The interscalene block can be performed with ultrasound, paresthesia, or nerve stimulation techniques to provide anesthesia and analgesia for the shoulder and proximal arm by targeting the brachial plexus’ roots at C5, C6, and sometimes C7 levels.
- Interscalene blocks are not recommended for forearm or hand surgeries as the inferior trunk is spared. The inferior trunk gives rise to the ulnar nerve (C8-T1), which provides sensory innervation to the medial one-and-a-half fingers and ulnar half of the palm; medial brachial cutaneous nerve (T1), which provides sensory innervation to the skin of the arm; and medial antebrachial cutaneous nerve (C8-T1) which provides sensory interaction to the skin of the forearm.
- Hemidiaphragmatic paralysis and Horner syndrome are expected side effects of the block.
Anatomy
- The interscalene block targets the ventral rami of C5, C6 (often seen split into two distinct neural structures), and sometimes C7 at the upper roots of the brachial plexus (C5-T1). As the nerves exit the intervertebral foramina, they travel anterolaterally and inferiorly and pass between the anterior and middle scalene muscles.1
- The area between the anterior and middle scalene muscles is referred to as the “interscalene groove” and is the target of the interscalene block. It is lateral to the anterior scalene muscle and medial to the middle scalene muscle.1
- The interscalene groove is found lateral to the internal jugular vein, carotid artery, and vertebral artery.
- The nerves can form a pattern on ultrasound, colloquially referred to as the “stoplight sign.”
Patient Positioning
- The most ergonomic position for the interscalene block is semi-supine, with the ipsilateral side up and the patient’s head turned to the contralateral side.
- Other positions that can be used to achieve an interscalene block include supine and semi-lateral decubitus, with the ipsilateral side slightly raised.

Figure 1. Patient position and ultrasound position commonly used for interscalene block. Image courtesy of Vats Ambai, MD.
Needle Positioning
Ultrasound Technique
- With the patient in the optimum position and head turned in the opposite direction, a linear high-frequency ultrasound probe is placed transversely along the neck, approximately 2–4 cm cephalad to the clavicle in the supraclavicular fossa, at the level of the cricoid cartilage.
- The target nerves appear as hypoechoic structures between the anterior and middle scalene muscles. The number of nerves seen ranges from 3 to 5, depending on the individual’s anatomy.1,2
- Color-doppler can be used to identify and avoid vasculature in the field.
- An alternative approach to establishing the interscalene view is to start with the supraclavicular brachial plexus view and translate the probe cephalad until the plexus coalesces to form a series of hypoechoic structures between the anterior and middle scalene muscles.
- Once the interscalene view has been confirmed and the entry point has been anesthetized, a block needle can be guided to the interscalene groove using either an in-plane or an out-of-plane technique. The in-plane technique involves the needle entering laterally and traveling medially through the middle scalene muscle before exiting the middle scalene fascia until it lies adjacent to the lateral side of the interscalene groove. The out-of-plane technique can be achieved by guiding the needle between the anterior and middle scalene muscles to the interscalene groove.1
- The needle passage through the middle scalene fascia sometimes produces a tactile or visual effect for the provider.
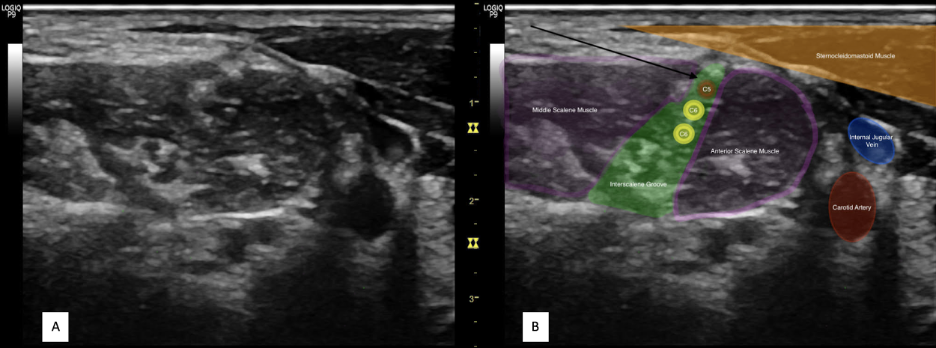
Figure 2. A) Ultrasound view of Interscalene block. B) Overlay of Figure 2A. The arrow depicts an example of a common needle trajectory for the interscalene block. Image courtesy of Vats Ambai, MD.
Nerve Stimulation Technique
- Nerve stimulation, particularly when combined with ultrasound, can help identify nerves at risk of needle trauma. The long thoracic and dorsal scapular nerves commonly pass through the middle scalene muscle and should be carefully avoided to prevent injury (Figure 3).
- With the patient in the optimum position and their head turned in the opposite direction, the posterior border of the sternocleidomastoid is palpated and followed posterolaterally to find the interscalene groove between the bellies of the anterior and middle scalene muscles. A line can be traced laterally from the cricoid cartilage to the interscalene groove, which usually corresponds to the C6 vertebrae. These reference points are typical insertion points for the interscalene block.1-3
- After local anesthesia has been established at the intended entry point, an insulated stimulating needle with initial current settings of 1-2 mA, pulse duration of 0.1 ms, and a frequency of 2 Hz can be inserted at a slightly caudad angle and advanced in-plane from posterior to anterior. The needle is advanced until a motor response is generated in the distribution of the C5-C6 nerve roots, as demonstrated by muscular contraction of the deltoid, biceps, or brachioradialis.1 Avoid eliciting a motor response below 0.2 mA, as this may suggest intraneural needle placement and result in a posttraumatic inflammatory response.4
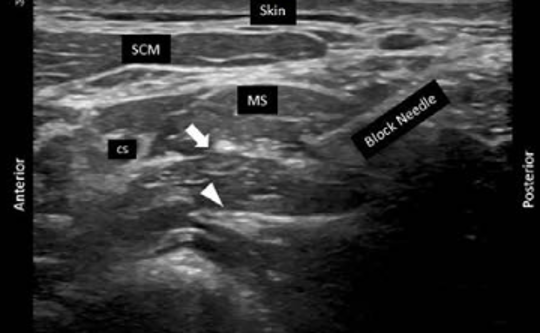
Figure 3. Location of dorsal scapular (arrow) and long thoracic (arrowhead) nerves in the middle scalene muscle. SCM = sternocleidomastoid muscle; MS = middle scalene muscle; C5 = 5th cervical nerve root. Used with permission from Gürkan Y, et al. A A Practice. 2024.6
Considerations
Injectate Volume
- Typical volumes used range from 10-20 mL when performed under ultrasound guidance, and up to 40 mL for non-ultrasound-guided techniques.
- A catheter may also be placed for prolonged delivery of local anesthetics and extended analgesia.
- Hydrodissection with nonactive fluid, such as normal saline, is recommended to ensure proper needle placement and to minimize unnecessary local anesthetic loss. Negative aspiration should also be confirmed prior to injection and intermittently upon administering the local anesthetic.
Side Effects
- The phrenic nerve lies along the anterior surface of the anterior scalene muscle, deep to the sternocleidomastoid, which is routinely blocked with this technique. Ipsilateral blockade of the phrenic nerve leads to hemidiaphragmatic paralysis, which may not be tolerated in patients with pulmonary disease, obesity, or uncontrolled anxiety.1
- Ipsilateral Horner syndrome can result from blockade of the cervical sympathetic chain, leading to ptosis, miosis, anhidrosis, conjunctival injection, and nasal congestion.1
Complications1-3
- Potential complications should be considered when performing the interscalene block: infection, bleeding, nerve damage (including spinal cord, spinal nerves, brachial plexus, and the long thoracic and dorsal scapular nerves as they pass through the middle scalene muscle; avoid injection against high resistance [> 15 psi] to minimize risk5); arterial injection (including the vertebral artery as it passes deep to the anterior scalene muscle or branches of the thyrocervical trunk); epidural or intrathecal injection (avoid advancing needle more than 2.5 cm to minimize risk); pneumothorax, medication reaction, and localized pain at the site of injection.
Technique Comparison
- When comparing ultrasound to nerve stimulation technique, ultrasound allowed for fewer needle passes and faster onset of motor blockade after injection. However, there were no clinically significant differences in block failure, patient satisfaction, or complications.2
- When comparing nerve stimulation to paresthesia-based techniques, there were no clinically significant differences in onset time, block failure, patient satisfaction, or complications.3
References
- Urmey W. Chapter 45 Brachial Plexus Block. In: Yao & Artusio’s Anesthesiology: Problem-Oriented Patient Management. Wolters Kluwer Health/Lippincott Williams & Wilkins; 2012:1028-32.
- Liu S, Zayas, V; Gordon, MA et al. A prospective, randomized, controlled trial comparing ultrasound versus nerve stimulator guidance for interscalene block for ambulatory shoulder surgery for postoperative neurological symptoms. Anesth Analg. 2009; 109(1): 265-71. PubMed
- Liguori GA, Zayas VM, YaDeau JT et al. Nerve localization techniques for interscalene brachial plexus blockade: A prospective, randomized comparison of mechanical paresthesia versus electrical stimulation. Anesth Analg. 2006; 103(3): 761-7. PubMed
- Steinfeldt T, Graf J, Schneider J, Nimphius W, Weihe E, Borgeat A, Wulf H, Wiesmann T. Histological consequences of needle-nerve contact following nerve stimulation in a pig model. Anesthesiol Res Pract. 2011; 2011:591851. PubMed
- Gadsden JC, Choi JJ, Lin E, Robinson A. Opening injection pressure consistently detects needle-nerve contact during ultrasound-guided interscalene brachial plexus block. Anesthesiology. 2014;120(5):1246-53. PubMed
- Gürkan Y, Şimşek D, Güllü B, et al. Selective dorsal scapular nerve and long thoracic nerve blocks for rescue analgesia in scapulothoracic arthrodesis surgery: A case report. A A Practice. 2024; 18 (3): e01765. PubMed
Copyright Information

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.